Diets with fewer calories potentially elevate the risk of depression.
Revamped Article:
- Diving into the impact of diets on depression symptoms: A groundbreaking cross-sectional study, led by researchers from the bustling metropolis of Toronto, Canada has illuminated potential risks associated with popular weight loss techniques.
- Peeling back the layers on dieting and mental health: The researchers delved into whether specific types of diets could inadvertently exacerbate mental health issues, specifically depression.
- The new kid on the block in weight loss strategies: In today's health-conscious world, many Americans - approximately 93% according to recent guidelines - are grappling with either obesity or being overweight. Ranging from altering dietary habits to using medications, an array of weight loss methods are up for grabs.
One common pitfall faced by those aiming to shed pounds is overzealous calorie or nutrient restriction. The suggested approach involves slashing 500 to 1,000 calories per day to lose 1 to 2 pounds weekly. Simple food substitutions and avoiding sugary beverages can pack a punch in this effort.
However, many dieters take things to the extreme by radically cutting their calorie intake or focusing on a single food group, like the carnivore diet.
While embracing weight loss is crucial for some individuals, it's equally important to approach it sensibly. Overly restrictive or extreme dieting methods have been known to give rise to physical health issues, and the present study aims to shed light on potential mental health implications.
Their findings were published in BMJ Nutrition Prevention & Health.
Linking Diet and Mental Health
Depression, a relentless mental health foe, affects countless individuals every year, with the U.S. witnessing a rise in reported cases. Data from 2020 indicates that as many as 18.4% of American adults have received a diagnosis for depression [*].
The research team cited evidence suggesting that embracing a balanced, nutritious diet can bolster mental health, while processed foods can cause detrimental effects [*]. However, they emphasized the need for more information on the repercussions of calorie and nutrient restriction - a gap their study aimed to address.
The researchers utilized data from 28,525 adults who took part in both the National Health and Nutrition Examination Survey (NHANES) and the Patient Health Questionnaire-9 (PHQ-9). NHANES provides information on health and nutrition, while the PHQ-9 helps evaluate depressive symptoms.
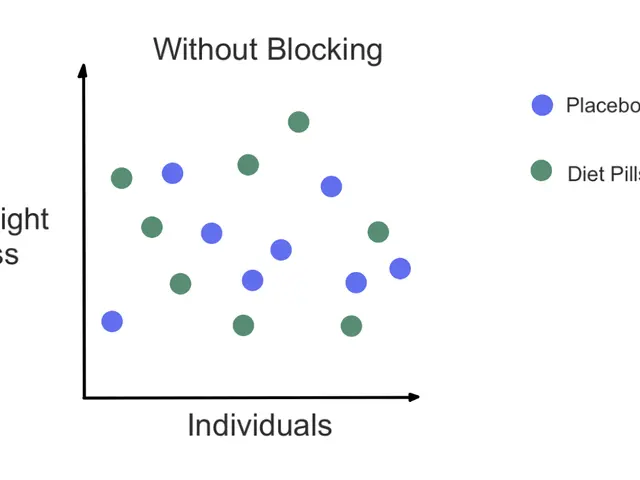
The participants were grouped into four categories:
- calorie-restricted diet (8%)
- nutrient-restricted diet (3%)
- established medical dietary patterns, like the DASH diet (2%)
- not following a diet (87%)
The researchers compared PHQ-9 responses among the participants, taking factors such as body mass index (BMI) and biological sex into account.
A Potential Red Flag: Men and Low-Calorie Diets
The researchers found a correlation between the diet category participants belonged to and their depressive symptoms. Overall, 7.79% of the participants reported experiencing depressive symptoms [*].
Individuals who adhered to calorie-restricted diets demonstrated higher overall PHQ-9 scores, with an average increase of 0.29 points compared to the other groups []. This trend was more apparent among participants with higher BMIs in the calorie-restriction group, whose PHQ-9 score was elevated by an average of 0.46 points [].
An even more worrisome association emerged among overweight individuals following nutrient-restricted diets. Although the nutrient-restriction group did not show an increased PHQ-9 score on average, overweight participants in this group exhibited a higher PHQ-9 score of 0.61 points [*].
Further analysis revealed some associations varying by the participants' biological sex. The researchers used the PHQ-9 to assess somatic symptoms - physical symptoms linked to psychiatric distress [*].
Bloke-centric Troubles:
"In biological men, all three dietary patterns were associated with higher somatic symptom scores," according to the study authors [*]. Men who adhered to nutrient-restricted diets were also more likely to experience an increase in cognitive-affective symptoms.
The researchers speculate that these connections might be linked to men having higher caloric needs and not obtaining adequate nutrition via their dietary intake.
The Mysterious Link between Calorie Restriction and Mental Health
Amy Roethler, a dietitian and nutritionist for Newport Healthcare's PrairieCare program, weighed in on the study's findings with Medical News Today.
"For many years, there has been suspicion that significant calorie restriction can lead to negative impacts on one's mental health, specifically depressive symptoms," she shared with MNT. "This study certainly provides additional support to this theory."
Roethler added that in her experience, dieters often focus more on restricting their calorie intake instead of paying attention to their nutrient intake - a common misstep that likely contributes to this issue.
"Typically, I find that once individuals start making changes to their eating habits, focusing on fruits, vegetables, whole grains, healthy fats, and lean proteins, they begin to feel better - often leading to sustained changes," she concluded.
Roethler recommended that primary care providers working with patients attempting to lose weight while battling depression refer their patients to registered dietitians for expert guidance.
Timothy Frie, a neuronutritionist and nutritional psychology researcher, also voiced his thoughts on the study, which he was not involved in, with MNT.
"The finding that calorie restriction is associated with increased depressive symptoms, particularly in men and individuals with higher BMIs, highlights that mental health consequences may arise when dietary changes are made without adequate support, monitoring, or nutrient sufficiency," Frie stressed.
He explained that calorie restriction can sometimes lead to individuals slashing essential foods for maintaining mood regulation:
"Reducing calorie intake or entire food groups results in nutritional deficiencies in B vitamins, iron, omega-3 fatty acids, and complex carbohydrates - all vital for neurochemical processes that regulate mood and emotions."
In conclusion, the research points to potential adverse mental health effects of calorie restriction, particularly for men and overweight individuals. As more studies delve into specific nutritional deficiencies related to depression occurring during weight loss attempts, it's crucial to approach dieting with caution and guidance from experts.
- The groundbreaking study conducted by Toronto researchers highlights the potential mental health risks associated with common weight loss methods.
- The study, published in BMJ Nutrition Prevention & Health, found a correlation between calorie-restricted diets and increased depressive symptoms.
- The research team stressed the need for further information on the effects of calorie and nutrient restriction on mental health.
- Overweight men following nutrient-restricted diets showed a higher likelihood of experiencing increased depressive symptoms.
- The study findings suggest that mental health consequences may arise when dieting without enough support, monitoring, or nutrient sufficiency.
- Adopting a balanced, nutritious diet, focusing on essential nutrients, may help alleviate depression symptoms and improve overall mental health.