Digestive issues: Symptoms, origins, and remedies
Functional dyspepsia is a common chronic digestive disorder that affects up to a significant portion of the population. Characterized by recurring upper abdominal pain or discomfort without visible stomach damage, this condition can be challenging to manage due to its multifactorial causes.
Symptoms of Functional Dyspepsia
Common symptoms of functional dyspepsia include upper abdominal pain, early fullness during meals, bloating, nausea, belching, and burning sensations. These symptoms can be distressing and impact quality of life, but there are several approaches to managing the condition.
Causes of Functional Dyspepsia
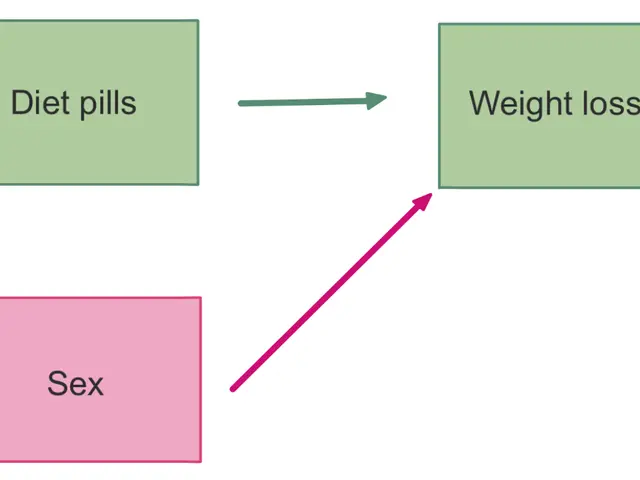
The causes of functional dyspepsia are complex and can vary among individuals. Factors such as genetic predisposition, prior viral infections, stress and psychological factors, inflammation or trauma, post-surgery effects, hormonal influences, abnormal gastric sensorimotor function, central nervous system dysfunction, and dietary habits can contribute to the development of the condition.
Lifestyle and Dietary Modifications
Lifestyle and dietary modifications play a fundamental role in managing functional dyspepsia symptoms. Eating smaller, more frequent meals instead of large ones can help reduce stomach distension. Avoiding trigger foods, particularly spicy, fatty, or acidic foods, may also help alleviate symptoms. Limiting alcohol and caffeine intake, eating slowly and chewing food thoroughly, staying hydrated, and regular exercise can also contribute to symptom management, though evidence for the latter is limited.
Medications
Pharmacological therapy is usually considered when lifestyle changes alone are insufficient. Prokinetic agents, which improve gastric emptying, are often prescribed to manage symptoms related to delayed stomach emptying. Acid suppression therapies, such as proton pump inhibitors and H2 blockers, are often prescribed if acid reflux or burning sensations accompany symptoms. Antiemetic agents are used to control nausea and vomiting when present.
Summary
In managing functional dyspepsia, lifestyle and dietary modifications play a crucial role, complemented by pharmacological treatments tailored to predominant symptoms. While lifestyle changes can help many patients substantially, medications are often required for symptom control, especially related to gastric motility and acid-related discomfort.
It's important to note that changes in medications should only be made under the supervision of a doctor due to potential drug interactions. For those experiencing severe or frequent symptoms, it is advisable to seek medical help promptly.
In April 2020, the Food and Drug Administration (FDA) requested that all forms of prescription and over-the-counter (OTC) ranitidine (Zantac) be removed from the United States market due to unacceptable levels of NDMA, a probable carcinogen. This underscores the importance of consulting a doctor or pharmacist when managing any digestive issues, including functional dyspepsia.
For those experiencing dyspepsia during pregnancy, it's essential to seek advice from a healthcare provider to ensure safe management strategies are employed.
References:
- Drossman, D. W., & Talley, N. J. (2016). Functional Gastrointestinal Disorders. Gastroenterology, 150(7), 1411-1420.
- Talley, N. J., & O'Morain, C. F. (2015). Functional Dyspepsia. The Lancet Gastroenterology & Hepatology, 2(3), 205-215.
- Talley, N. J., & Ford, A. C. (2017). Functional Dyspepsia. In A. C. Ford, M. E. Fett, A. S. Walker, & H. C. Whiting (Eds.), Gastrointestinal Disorders (pp. 146-159). Wiley-Blackwell.
- Talley, N. J., & Ford, A. C. (2013). Functional Dyspepsia. In A. C. Ford, M. E. Fett, A. S. Walker, & H. C. Whiting (Eds.), Gastrointestinal Disorders (pp. 146-159). Wiley-Blackwell.
- Predictive factors for functional dyspepsia severity can include psychological distress and a history of irritable bowel syndrome, suggesting the need for comprehensive mental health evaluations and therapies.
- Given the multifactorial causes of functional dyspepsia, a personalized treatment approach is often necessary, incorporating science-backed therapies and treatments, medical-conditions like stress management, and self-development strategies.
- Along with pharmacological and lifestyle interventions, nutrition plays a vital role in managing functional dyspepsia symptoms. This may involve weight management and a focus on digestive health through dietary modifications.
- In addition to traditional treatments, some patients may find relief in alternative therapies such as CBD oil, which has been shown to reduce symptoms of anxiety and inflammation, although more research is needed to fully understand its benefits.
- People living with multiple medical-conditions like COPD, asthma, psoriatic arthritis, or sclerosis may be at a higher risk for developing functional dyspepsia, emphasizing the importance of addressing digestive-health within the context of overall health-and-wellness.
- A large-scale review of studies found a higher prevalence of functional dyspepsia among those with type 1 and type 2 diabetes, potentially due to shared pathophysiological mechanisms like autonomic neuropathy and inflammation.
- Research has linked functional dyspepsia with an increased risk of peritonitis, a serious digestive complication, highlighting the importance of regular monitoring and prompt medical attention for those experiencing symptoms.
- HIV-positive individuals may be at a higher risk for developing functional dyspepsia due to gastrointestinal complications resulting from immune system dysregulation and medication side effects.
- Crohn's disease and ulcerative colitis, both forms of inflammatory bowel disease, can share similarities with functional dyspepsia, further underscoring the importance of proper care and education-and-self-development for effective management of all related conditions.
- Bipolar disorder and depression have been found to be more prevalent among those with functional dyspepsia, suggesting a potential connection between mental health and digestive health.
- As functioning dyspepsia can impact fitness-and-exercise performance and motivation, addressing digestive health and implementing weight management strategies may contribute to improved overall well-being and personal-growth.
- Geriatric patients managing functional dyspepsia might also require specialized care under Medicare guidelines.
- Patients with skin-care issues, such as dermatitis or psoriasis, may find that addressing digestive health can contribute to alleviating or preventing symptoms related to inflammation.
- A thorough understanding of functional dyspepsia and its link to various health concerns can empower patients to advocate for themselves, seek appropriate care, and make informed decisions about their treatments and Medication usage.
- It is important to remember that education and self-development play a crucial role in managing any health-related condition, including functional dyspepsia.
- In conclusion, understanding functional dyspepsia and its multifactorial causes, as well as exploring various lifestyle, dietary, and therapeutic approaches, can lead to more effective symptom management and improved quality of life for affected individuals.