During Slumber, Your Brain Performs Garbage Collection - Discovering the Consequences if this Process Fails
Sleep, a period often perceived as passive rest, is in fact a time of active biological maintenance for the brain. The intricate machinery of consciousness undergoes essential servicing during this nightly reprieve, thanks to the brain's remarkable nocturnal maintenance system [1].
At the heart of this system lies the glymphatic pathway, a waste clearance network unique to the brain. This system plays a critical role in brain maintenance during sleep, clearing metabolic waste products, including toxic proteins such as beta-amyloid and tau, which are implicated in neurodegenerative diseases like Alzheimer's [2].
Aquaporin-4 (AQP4) water channel proteins, strategically positioned along the walls of blood vessels in the brain, are crucial for the glymphatic system's effectiveness [3]. During sleep, especially the slow-wave phase of non-REM (NREM) sleep, brain neural activity patterns and vascular pulsations enhance cerebrospinal fluid (CSF) movement through the glymphatic pathways, promoting interstitial fluid (ISF) exchange and clearance of neurotoxic waste [4].
Environmental factors significantly impact sleep architecture, with bedroom temperature ideally remaining between 60-67°F (15-19°C) for quality slow-wave sleep [5]. Preservation of glymphatic function ensures the removal of beta-amyloid and tau proteins, reducing their accumulation and thereby mitigating pathological mechanisms underlying Alzheimer's and Parkinson’s diseases [1][3].
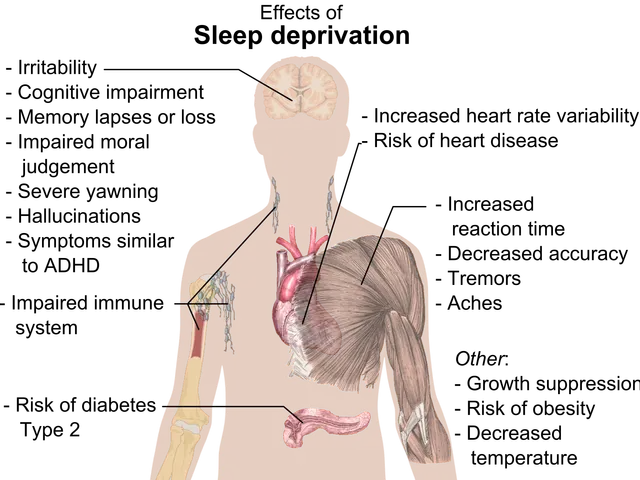
The efficiency of the glymphatic system has direct effects on cognitive function. Disturbances in sleep, such as fragmentation or disruption of slow-wave activity, can impair glymphatic clearance, leading to the buildup of toxic proteins that contribute to neuronal damage and cognitive decline [6]. Moreover, vascular and blood-brain barrier dysfunction, which may involve specialized vascular cells called pericytes, also interact with sleep quality to influence cognitive trajectories and dementia risk in aging populations [2].
Dysfunction in GABAergic interneurons, especially in individuals with genetic vulnerabilities like APOE ε4, further disrupts slow-wave sleep and glymphatic activity, compounding risk for neurodegeneration [3].
For healthcare systems, sleep assessment gains importance as preventative neurology, with detecting and addressing sleep disruptions early potentially representing among the most cost-effective interventions for reducing long-term neurological disease burden [7]. The glymphatic system's sleep-dependent nature helps answer the evolutionary question of why sleep exists, suggesting that sleep evolved because consciousness and waste clearance cannot effectively coexist [8].
Advanced MRI techniques using contrast agents allow direct observation of glymphatic function in living subjects [9]. Astrocytes, star-shaped glial cells, form the structural foundation of the glymphatic system [10]. The glymphatic system facilitates the removal of proinflammatory cytokines, glucose, lipids, amino acids, and growth factors during sleep [11].
Pharmaceutical interventions targeting glymphatic enhancement show early promise, with compounds that safely enhance cerebrospinal fluid production, reduce brain cell adhesion during sleep, or improve AQP4 channel function potentially providing breakthrough treatments for various neurological conditions [12].
Personalized sleep optimization protocols based on individual glymphatic function measurement represent an exciting frontier in sleep research [13]. Dietary patterns influence glymphatic function both directly and through sleep quality effects, with evidence suggesting intermittent fasting approaches may enhance waste clearance [14].
In evolutionary brilliance, what appears as dormancy masks the brain's most sophisticated self-preservation mechanisms at work [15]. The glymphatic system, a brain-specific waste clearance network, increases its activity by 1,000% during sleep [16]. The glymphatic system shows particular activity during slow-wave sleep, the deepest non-REM sleep phase [17].
Brain-computer interface technologies under development could potentially monitor and enhance slow-wave activity during sleep without disrupting sleep continuity [18]. Light exposure management is crucial—even brief exposure to blue light from electronic devices can reduce slow-wave sleep quality [19]. Sleep doesn't simply refresh the mental state; it literally washes the brain clean [20].
Chronotherapeutic approaches—treatments timed to biological rhythms—show particular promise for glymphatic enhancement [21]. Two-photon microscopy in animal models permits real-time observation of glymphatic function at the cellular level [22]. For individuals, prioritizing sleep continuity, creating sleep-supportive environments, addressing sleep disorders promptly, and maintaining consistent sleep timing represent practical strategies for enhancing glymphatic function [23].
Certain polymorphisms in the AQP4 gene correlate with increased risk for neurodegenerative diseases, including Alzheimer's [24]. A landmark 2013 study documented cerebrospinal fluid surging through brain tissue during sleep, removing toxic waste proteins like beta-amyloid [2]. Positron emission tomography (PET) scanning with specialized tracers enables tracking of specific waste products like beta-amyloid and tau proteins [25].
In summary, the glymphatic system's role in waste clearance during sleep is essential for preserving brain health, supporting memory consolidation, and reducing the risk of neurodegenerative diseases. Impaired glymphatic clearance due to poor sleep quality or neurovascular dysfunction is strongly associated with cognitive decline and the pathology of conditions such as Alzheimer's disease [1][2][3].
Technology and science have uncovered a remarkable self-preservation mechanism in sleep, as the glymphatic system, a brain-specific waste clearance network, increases its activity by 1000% during this period [16]. This system plays a critical role in health and wellness, mental health, and even the prevention of neurodegenerative diseases such as Alzheimer's and Parkinson’s, by clearing metabolic waste products, including toxic proteins [1, 2]. Advanced MRI techniques and pharmaceutical interventions are being developed to monitor and enhance glymphatic function, offering potential breakthrough treatments for various neurological conditions [9, 12].