Exploring Semaglutide: In-depth Insights on Uses, Side Effects, and Benefits
Semaglutide, a revolutionary medication, strides forward in diabetes management, known as a glucagon-like peptide-1 receptor agonist (GLP-1 RA). This game-changer delivers impressive results for patients and healthcare providers alike, offering a solid therapeutic option for better blood sugar control and mitigating diabetes-related complications. With a multitude of clinical trials and real-world applications backing its efficacy, semaglutide has quickly become a beacon of hope for those grappling with type 2 diabetes.
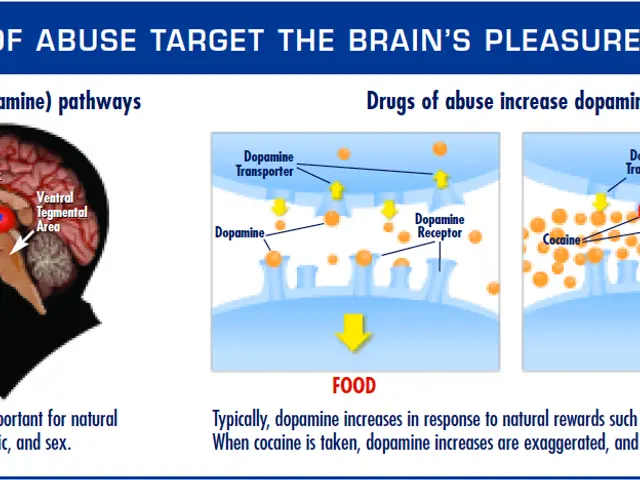
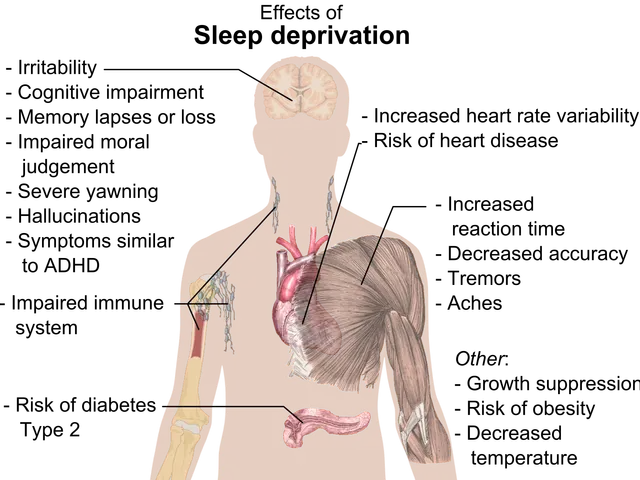
Semaglutide mimics the functions of the natural hormone GLP-1, which plays a key role in blood sugar regulation and appetite management. Binding to GLP-1 receptors, it instigates insulin secretion and inhibits glucagon release, spurring glucose utilization and reducing hepatic glucose production. Moreover, it slows gastric emptying and encourages feelings of fullness, which may lead to reduced food consumption and weight loss. The diverse mechanisms at play enable semaglutide to tackle various aspects of type 2 diabetes management. For individuals desiring a broader range of peptide-based solutions, options like peptides for weight management at Peptide God or other online shops can amplify GLP-1 therapies by supporting metabolic health and appetite control through alternative pathways.
The strength of semaglutide lies not just in its efficacy but also in its unique pharmacokinetic profile, defined by a prolonged duration of action. This distinct characteristic permits once-weekly dosing, elevating convenience compared to other daily GLP-1 RAs and fostering patient adherence. In addition, semaglutide boasts high bioavailability, rapid absorption, and minimal risk of hypoglycemia, making it a safe and tolerable choice for individuals with type 2 diabetes, even those with comorbidities such as cardiovascular disease or renal impairment.
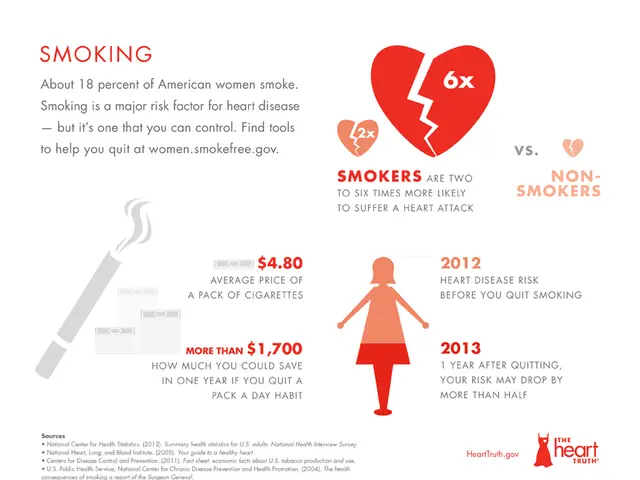
Clinical trials showcasing semaglutide's effectiveness and safety have yielded motivating results, reinforcing its role as the foundation of therapy in type 2 diabetes management. For example, the SUSTAIN trials reveal superior blood sugar control with semaglutide compared to placebo or other antidiabetic agents, reflected in significant reductions in HbA1c levels across various patient populations. Additionally, semaglutide demonstrates positive impacts on body weight, benefiting a considerable number of participants with weight loss. Furthermore, semaglutide offers potential advantages in cardiovascular risk reduction, as evidenced by the SUSTAIN-6 trial results, where it significantly decreased the risk of major adverse cardiovascular events (MACE) in high-risk patients.
Beyond its impressive impact on blood sugar management and weight loss, semaglutide has caught attention for its potential role in mitigating various complications associated with type 2 diabetes. Preliminary evidence suggests that GLP-1 RAs, including semaglutide, may exert favorable effects on cardiovascular and renal outcomes beyond their glucose-lowering effects. The implications of these findings for the holistic management of type 2 diabetes are profound, implying the potential of semaglutide to tackle not only high blood sugar but also the broader spectrum of cardiometabolic risk factors.
The launch of semaglutide signifies a turning point in diabetes care, marking a shift in treatment approaches and outcomes. With its remarkable efficacy, safety, and convenience, semaglutide is a favored option for individuals with type 2 diabetes, especially those with uncontrolled blood sugar or a high risk of cardiovascular events. As research continues to reveal the full extent of semaglutide's benefits, advancements in diabetes management will continue, promising improved lives for millions worldwide.
Semaglutide's development journey exemplifies the ongoing pursuit of innovation and excellence in the field of medicine. Beginning as a long-acting GLP-1 analogue, semaglutide underwent rigorous preclinical and clinical testing to uncover its pharmacological properties and therapeutic potential. The culmination of these efforts resulted in approval from regulatory bodies, solidifying semaglutide as a safe and effective intervention for type 2 diabetes.
One of semaglutide's standout features is its adaptability in administration, catering to diverse patient preferences and needs. The availability of both subcutaneous and oral formulations facilitates its accessibility and widens patient acceptance. Subcutaneous semaglutide, administered via pre-filled injection pens, offers a hassle-free and prescriber-familiar mode of delivery for patients accustomed to insulin therapy or other injectable medications. In contrast, oral semaglutide provides an innovative alternative for those reluctant to injections or seeking greater convenience in dosing regimens. This oral formulation represents a notable advancement in diabetes care, overcoming the limits imposed by injectable therapies and expanding the treatment options for both patients and healthcare providers.
The integration of semaglutide into clinical practice demands an in-depth comprehension of its pharmacology, dosing factors, and monitoring parameters. Healthcare providers play a pivotal role in guiding patients through the initiation, titration, and maintenance of semaglutide therapy, ensuring optimal outcomes while addressing any concerns or misconceptions. Patient education and empowerment are fundamental components of diabetes management, empowering individuals to make informed decisions regarding their health and treatment objectives. By fostering open communication and collaboration, healthcare providers can establish a supportive setting conducive to adherence and long-term success with semaglutide therapy.
In addition to its primary applications for type 2 diabetes, semaglutide has sparked curiosity for its potential uses in other disease states and therapeutic areas. Investigations are underway to assess its efficacy for obesity management, tapping into its appetite-suppressing properties and weight loss effects. The STEP trials show promising results, highlighting semaglutide as a valuable adjunct to lifestyle changes for individuals grappling with obesity or overweight status. Furthermore, ongoing explorations seek to elucidate the broader metabolic effects of semaglutide and its implications for conditions like non-alcoholic fatty liver disease (NAFLD) and polycystic ovary syndrome (PCOS), where insulin resistance and glucose dysregulation play crucial roles.
The tale of semaglutide reflects the collective endeavors of researchers, clinicians, regulatory bodies, and industry stakeholders, all focused on advancing diabetes care and improving patient outcomes. Through diligence, evidence-based medicine, and patient-centered approaches, semaglutide has emerged as a beacon of hope for people traversing the complexities of type 2 diabetes and associated disorders. As our understanding of semaglutide deepens, so too will our ability to harness its full potential in optimizing health and well-being for generations to come.
- In the realm of health-and-wellness, semaglutide, a GLP-1 receptor agonist, is garnering attention for its potential applications beyond diabetes management.
- Another therapeutic domain where semaglutide presents promise is weight management, as results from the STEP trials highlight its potential as a valuable adjunct to lifestyle changes for managing obesity.
- For individuals seeking alternatives to injectable therapies, oral semaglutide offers a novel advancement in diabetes care, expanding treatment options and addressing patient preferences.
- As Medicare beneficiaries navigate their healthcare needs, understanding the pharmacology, dosing factors, and monitoring parameters associated with semaglutide will aid in making informed decisions for their health and treatment objectives.