Fatigue Syndrome Chronic: Causes, Symptoms, and Treatment Options
Chronic Fatigue Syndrome: Taking a Deep Dive into the Mysterious Illness
Chronic Fatigue Syndrome (CFS), or Myalgic Encephalomyelitis (ME), is a long-lasting and complex condition that affects numerous body systems. Individuals afflicted by CFS often struggle with severe fatigue, sleep issues, cognitive problems, and a host of other symptoms, leading to a significant impact on their daily lives. Approximately 836,000 to 2.5 million Americans could be CFS sufferers, with up to 90% remaining undiagnosed.
Dr. Adam Staten, a general practitioner and clinical director at One Day Tests, explains that CFS remains a enigmatic and infuriating condition despite its common occurrence. He notes that research communities worldwide are gradually shedding light on its origin.
Core Symptoms of CFS
According to the Centers for Disease Control and Prevention (CDC), a diagnosis of CFS requires all three primary ("core") symptoms, as well as at least one secondary symptom:
Primary Symptoms:
- Prolonged Fatigue: Marked by substantial reductions in activity levels lasting for at least six months, the fatigue doesn't stem from unusually strenuous activity, is not alleviated by sleep or rest, and was not previously an issue.
- Post-exertional malaise (PEM): It's the worsening of symptoms after physical or mental activity that wouldn't ordinarily cause problems. Recovery from a relapse may take days, weeks, or even longer.
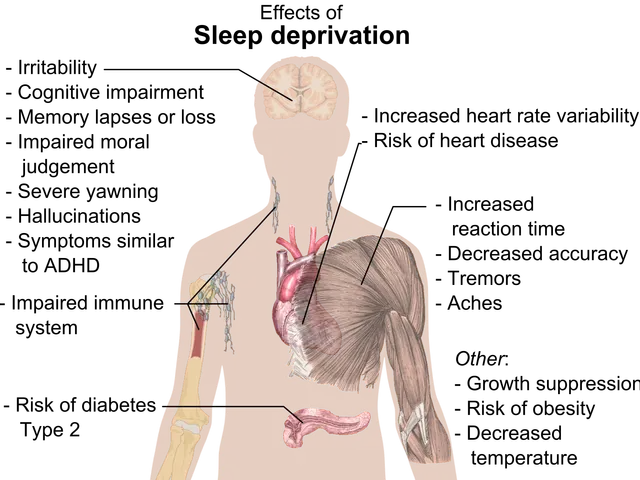
- Sleep Issues: Despite a full night's rest, patients may still feel weary and unrested. Some experience difficulties falling asleep or staying asleep.
Secondary Symptoms:
- Thought Processing Issues: Difficulties with thinking quickly or clearly, trouble with memory, and poor attention to details.
- Orthostatic Intolerance: This presents as worsening of symptoms when standing or sitting upright, often resulting in feelings of lightheadedness, dizziness, and weakness.
Other frequent CFS symptoms, as indicated by the CDC, include:- Pain (muscle pain, joint pain, and headaches)- Swollen lymph nodes in the neck or armpits- Frequent sore throat- Digestive problems, such as irritable bowel syndrome- Chills and night sweats- Food sensitivity and allergies, as well as sensitivities to light, odors, chemicals, or noise- Muscle weakness- Shortness of breath- Irregular heartbeat
CFS is most common in individuals aged 40 to 60, and women are more frequently affected than men. Nonetheless, anyone can develop this condition, the CDC stresses.
Delving into the Causes of CFS
While CDC researchers admit that the cause (or causes) of CFS is (are) still unclear, they suggest multiple possibilities. Some theories propose that CFS has several causes, including:
Infection
Whether chronic viral infection could be the root of CFS has long been debated. Staten points out that studies from the early 80s showed a link between the Epstein Barr virus (which causes mono) and prolonged symptoms of malaise and fatigue. However, no definitive link between CFS and infectious agents has been confirmed, leaving the role of viral and bacterial infections uncertain.
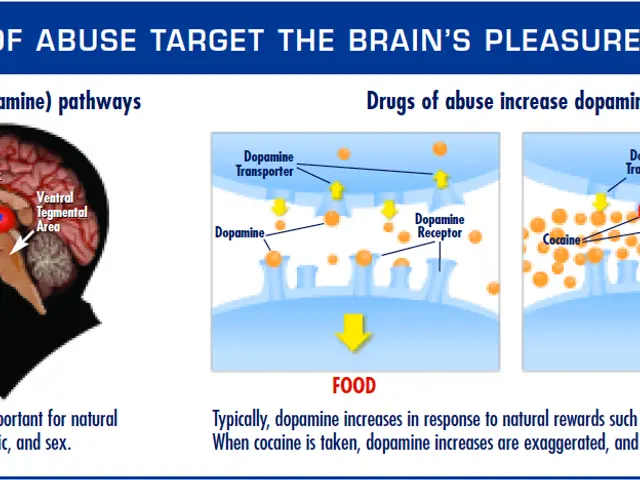
Immune System Dysregulation
There is substantial evidence supporting the theory that some instances of CFS are caused by autoimmune responses gone awry. Researchers have been able to demonstrate that certain autoantibodies appear more frequently in CFS sufferers, which has fueled speculation that CFS may be an autoimmune condition triggered by infection.
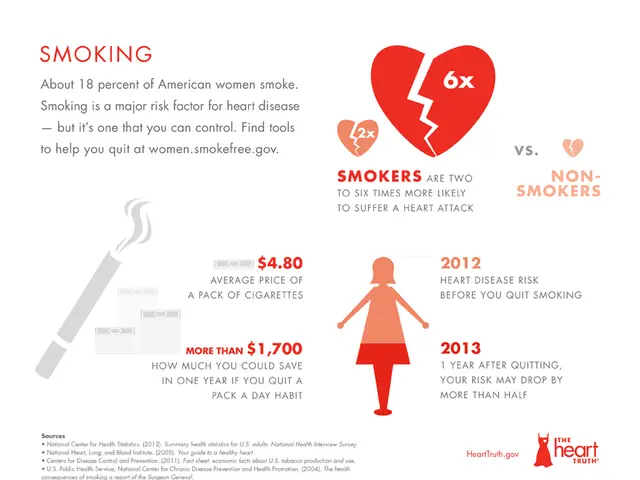
Cardiovascular
Studies have shown that patients with CFS often have abnormalities in their cardiovascular systems, such as reduced stroke volume. Low oxygen consumption in the lungs also seems to be a distinctive characteristic of CFS. Abnormalities could account for symptoms like dizziness on standing and irregular heartbeat, though further evidence is necessary to corroborate this association.
Genetics
Studies have revealed that 199 genetic alterations across 14 genes are present in 91% of CFS cases. Many of these genes play a crucial role in regulating mechanisms suspected to play a part in CFS, such as vulnerability to infection and impaired energy metabolism.
Neurological
MRI studies have shown structural changes in the brains of CFS patients, along with abnormalities in brain connectivity. CFS sufferers also tend to have impaired blood flow in the brain and increased intracranial pressure. These mechanisms may explain symptoms like brain fog, cognitive impairment, and headaches.
It is possible that the confusion surrounding the causes of CFS will one day give way to a better understanding of this condition, potentially leading to more targeted treatment strategies. For now, the medical community continues to investigate and learn about ME/CFS.
Diagnosing CFS
Since there are no lab tests or markers for CFS, diagnosis relies on ruling out other potential causes. A doctor will examine the patient's medical history and conduct physical and mental examinations, as well as ordering blood, urine, or other tests. Patients may be asked to keep a journal of their activities, too. The complexity of diagnosing CFS is increased by the fact that symptoms mimic those associated with numerous illnesses and that CFS typically presents with periods of remission and relapse. Due to symptom variation, medical professionals may find it challenging to identify cases of CFS.
Treating CFS
While there is no cure or medication for CFS, symptoms can be managed to some extent. Patients, their families, and healthcare providers should collaborate to prioritize the issue causing the most problems and treat it first, discussing the potential benefits and disadvantages of particular treatment plans. Because of the intricacy of CFS, patients are typically managed by multidisciplinary teams. Addressing a patient's mental health is vital for managing CFS symptoms, as stress, anxiety, and depression can exacerbate physical symptoms. Supporting patients' mental health is one of the keys to managing their symptoms.
Despite various theories and ongoing research, the elusive cause (or causes) of CFS remains an unresolved mystery. As the medical community continues to investigate, the search for answers is still on for those affected by this enigmatic condition. For more information, consult resources such as the Mayo Clinic and the Solve ME/CFS Initiative (Solve M.E.).
- CFS, or Chronic Fatigue Syndrome, is a complex medical-condition that often involves sleep issues, cognitive problems, and prolonged fatigue, which can significantly impact an individual's daily life.
- To diagnose CFS, healthcare providers rely on the patient's medical history, physical and mental examinations, and ruling out other possible causes, as there are no specific lab tests or markers.
- Treatment for CFS focuses on managing symptoms, such as mental health issues, fitness and exercise, nutrition, and in some cases, CBD, to improve the overall health and wellness of the individual.
- While the origins of CFS remain unclear, ongoing research suggests multiple possibilities like chronic viral infections, immune system dysregulation, genetic factors, cardiovascular abnormalities, and neurological causes.