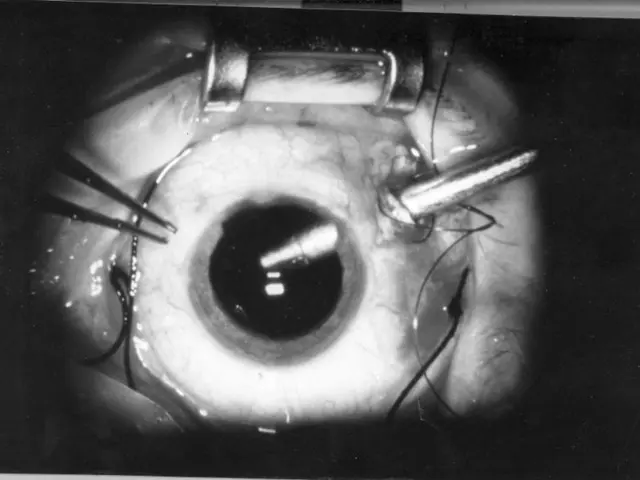
Gum Surgery Preparation, Procedural Details, and Post-Operative Care
Periodontal surgery, a specialized form of gum treatment, is primarily used to address the advanced stages and complications of gum disease. This surgery plays a crucial role in eradicating infection, restoring gum and bone health, and preserving teeth.
The conditions treated by periodontal surgery include advanced gum infections (periodontitis), deep periodontal pockets, gum recession, bone loss, and anatomical defects caused primarily by periodontal disease.
Periodontitis, a more severe form of gum disease, leads to bone and tissue damage, gum separation from teeth, and the development of pockets that trap bacteria and lead to infection. Surgery helps remove bacteria and tartar buildup from deep gum pockets, reduces pocket depth, restores lost tissue when possible, and halts disease progression.
Deep periodontal pockets and furcation involvement, which require pocket reduction or correction of anatomic defects, are another indication for periodontal surgery. Gum recession, often resulting in exposed sensitive tooth roots, is addressed through gum grafting techniques such as Free Gingival Graft, Subepithelial Connective Tissue Graft, and Acellular Dermal Matrix Allograft.
In severe cases of gum disease, surgical procedures like bone grafting are performed to restore lost bone and support the teeth. Other specific surgical treatments, like flap surgery, frenectomy, and peri-implantitis treatment for infected implants, may also fall under periodontal surgical care.
It is essential to note that if left untreated, gum disease may lead to the development of various health problems, such as cardiovascular disease, diabetes, and pre-term, low-birth-weight babies.
Recovery times will depend on the extent of the procedure, and people may require pain relief medications, use an antiseptic mouthwash, avoid strenuous exercise, eat soft foods, and not smoke. Proper oral hygiene, including seeking regular dental care, brushing and flossing two times a day, can reduce the risk and severity of gum disease.
On average, treatment of gum disease cost ranges from $500 to $10,000 depending on the type of surgery. The cost of dental procedures, including gum disease treatment, may or may not be covered by insurance, and it is essential to speak with an insurance carrier to discuss dental benefits.
Some gum surgery procedures may require a person to be asleep or partially asleep, while others only involve the use of a local anesthetic. Laser therapy is used by some dentists to reduce the size of pockets and restore damaged connective tissue, although no current evidence fully supports it.
In conclusion, periodontal surgery offers a comprehensive approach to treating advanced gum infections, deep pocketing, gum recession, bone loss, and anatomical defects caused primarily by periodontal disease. By addressing these issues, periodontal surgery contributes significantly to maintaining oral health and overall well-being.
- Beyond its primary role in addressing gum disease, predictive models could help anticipate the potential need for periodontal surgery among individuals with increased risk factors.
- Depression, a common mental-health condition, has been linked to the presence of periodontal disease, suggesting a need for workplace-wellness programs that address both mental and oral health.
- Medication used to treat medical-conditions like bipolar disorder or cancer may impact oralhealth by causing conditions such as xerostomia (dry mouth), potentially increasing the risk of periodontal disease.
- Science has shown a correlation between chronic diseases like diabetes and periodontal disease, highlighting the importance of regular medical-condition check-ups to ensure overall health and well-being.
- In regards to respiratory conditions like asthma, an improvement in cardiovascular-health through fitness-and-exercise and proper nutrition can help reduce the severity of symptoms and thus lower the chance of gum disease occurring.
- Digestive-health issues resulting from autoimmune-disorders like inflammatory bowel disease can negatively impact the immune system, making individuals more susceptible to periodontal infections.
- Eye-health is also crucial, as some conditions, such as dry eye or rheumatoid arthritis, can lead to an increased risk of developing periodontal disease.
- Hearing health should not be overlooked either, as sensorineural hearing loss, a common condition among the older population, has been associated with an increased risk for periodontal disease.
- With the rise in chronic diseases like obesity, the incidence of skin-conditions, such as acne or psoriasis, has also increased, potentially impacting skin-care and skincare-related medical procedures.
- Therapies-and-treatments for conditions like psoriasis or lupus, which affect the skin, may have side-effects that impact the oralcavity and, consequently, the need for periodontal care.
- Nutritional imbalances, especially deficiencies in vitamins like C or D, can negatively impact periodontal health, making it essential to maintain a balanced diet for overall health and wellness.
- In addition to periodontal surgeries for gum disease, therapies-and-treatments for related conditions such as dental-implants, root canals, and dental-crowns may also be necessary to ensure optimal oral and overall health.