Impact of Gut Microbiota on Emotional States, Judgment, and Psychological Well-being
The gut microbiome, a vast community of microorganisms residing in our digestive system, plays a significant role in shaping our mental health and cognitive function. This intricate relationship between gut bacteria and the brain is known as the microbiota-gut-brain axis.
Gut bacteria produce and modulate neurotransmitters, chemical messengers that regulate mood, motivation, anxiety, and stress response. Approximately 95% of the body's serotonin, a neurotransmitter crucial for emotional well-being, is produced in the gut with microbial assistance [1].
These gut microbes also influence cognitive processes by modulating synaptic plasticity, the brain's ability to adapt and form new neural connections. Research in bipolar disorder models shows distinct gut microbiota compositions correlate with cognitive impairments, and transplanting healthy microbiota can partially restore cognitive function and neuroplasticity [2].
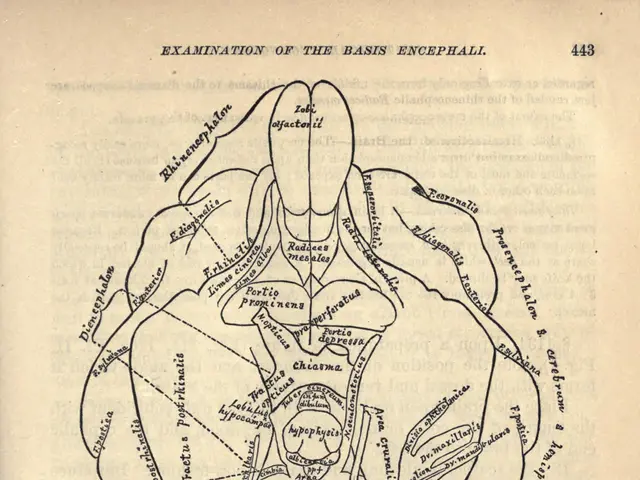
The gut microbiome exerts its influence through multiple pathways, including the blood-brain barrier, immune cells, and the vagus nerve, which serves as a high-speed information superhighway between the gut and brain [3].
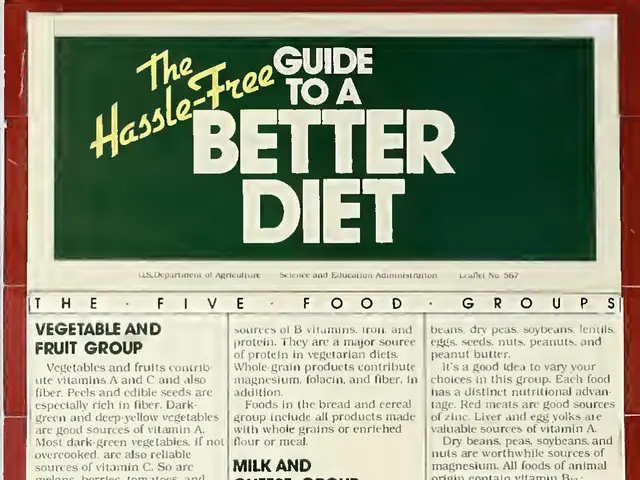
Diet and nutrition significantly impact the gut microbiome's diversity and health. Eating processed foods feeds bacteria that produce inflammatory compounds and crave more processed foods, while eating fermented foods and fiber feeds bacteria that produce mood-stabilizing compounds and crave healthier options [4].
Maintaining a healthy and diverse gut microbiome throughout life appears to protect against dementia and Alzheimer's disease [5]. Conversely, dysbiotic gut bacteria, those that produce inflammatory compounds, are associated with depression and cognitive deficits [6].
Research shows that transferring gut bacteria from depressed humans into germ-free mice causes the animals to develop depression-like behaviors [7]. This suggests that depression may actually be an inflammatory condition triggered by bacterial imbalances rather than a purely psychological disorder.
Traditional antidepressants may work for some people but not others, as they do not address the underlying microbial cause of depression. Emerging therapeutic approaches include probiotics, diet modifications, and microbiota transplantation, which have shown potential in improving mood disorders [8].
In summary, the gut microbiome influences mental health and cognition via biochemical signaling, modulation of brain plasticity, immune system interactions, and metabolic pathways. Understanding the gut-brain connection is revolutionary for those struggling with mood disorders, decision-making problems, or cognitive fog.
- The production of neurotransmitters, like serotonin, which plays a crucial role in emotional well-being, is largely modulated by gut bacteria.
- The gut microbiome, through multiple pathways such as the blood-brain barrier, immune cells, and the vagus nerve, exerts its influence over cognitive processes and mental health.
- A healthy and diverse diet, promoting the growth of bacteria that produce mood-stabilizing compounds, could potentially protect against mental health issues like depression and cognitive deficits.
- Novel therapeutic methods, such as probiotics, diet modifications, and microbiota transplantation, are showing promise in improving mood disorders, suggesting that addressing the gut-brain connection may revolutionize treatment for those struggling with mental health issues.