Individualized Approach to Lifestyle Factors May Reduce AFib Risk for Some People
Atrial fibrillation, the most widespread type of arrhythmia, affects individuals globally. This irregular heart rhythm condition is a significant risk factor for strokes. Beyond the known risk factors related to cardiovascular wellness, the occurrence of chronic conditions like cardiovascular, respiratory, metabolic, and mental health issues also increases the probability of atrial fibrillation.
The comprehensive management of atrial fibrillation goes far beyond medication for stroke prevention or rate or rhythm control. This complex disease is driven by numerous risk factors and comorbidities, making a multi-disciplinary, individualized approach critical for effective care.
Genetics, sex, and age are non-modifiable risk factors for atrial fibrillation, but lifestyle changes and medications aim to manage this condition effectively. Blood thinners or anticoagulants can reduce the risk of blood clot formation and stroke. Nonvitamin K antagonist oral anticoagulants (NOACs) have become the first-choice treatment for atrial fibrillation, outperforming traditional warfarin in some aspects.
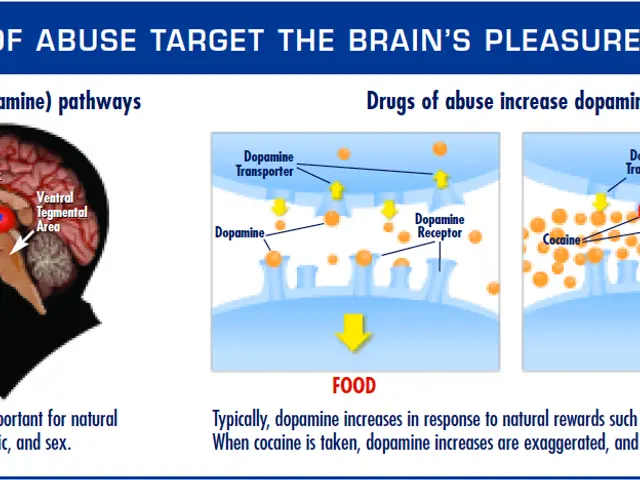
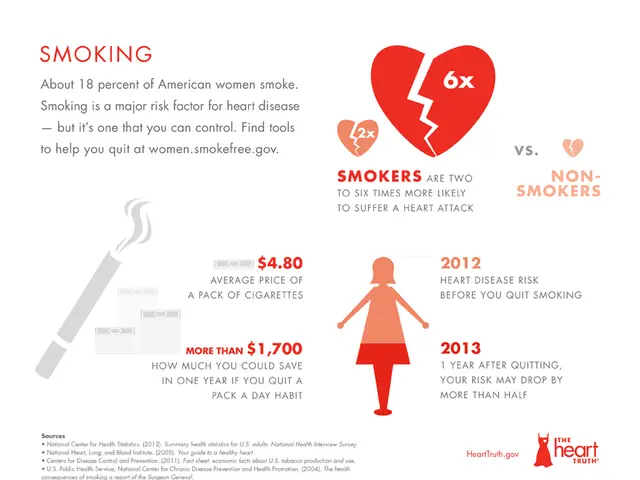
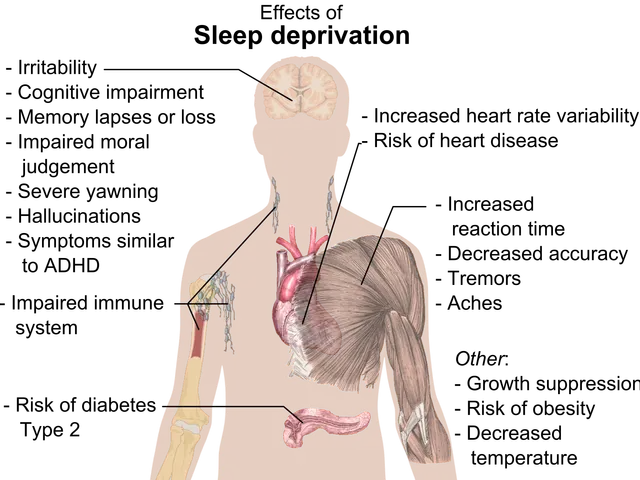
Physical inactivity, obesity, smoking, and excessive alcohol consumption increase the risk of atrial fibrillation incidence and symptom severity. Regular exercise, high-intensity interval training, and maintaining a healthy weight can lower the risk. Obstructive sleep apnea, characterized by the partial or complete obstruction of airways during sleep, heightens the risk of atrial fibrillation and its complications.
Hypertension, diabetes, coronary artery disease, and other cardiovascular conditions increase the risk of atrial fibrillation. Proper management of these comorbidities can help reduce the risk of atrial fibrillation recurrence and complications such as stroke. Notably, high total cholesterol and low-density lipoprotein levels are associated with a lower risk of atrial fibrillation, whereas higher levels of triglycerides elevate the risk.
Lifestyle changes, medications, and invasive procedures like catheter ablation are crucial for restoring a normal heart rhythm in individuals with atrial fibrillation. Other drugs, such as beta-blockers and calcium channel blockers, can control the heart rate. For those resistant to lifestyle modifications and medicines, catheter ablation may be an effective alternative.
Elevated blood pressure, obesity, unhealthy sleep patterns, high alcohol intake, unhealthy diets, smoking, and poor mental health are all associated with increased atrial fibrillation risk. Modifications in these areas can lead to a lower risk of atrial fibrillation incidence and burden.
Dr. Stephen Tang, a cardiac electrophysiologist, explained that many traditional cardiovascular risk factors, such as poor diet, physical inactivity, and obesity, are the same as those for atrial fibrillation, making their management challenging. Nevertheless, adopting healthy lifestyle behaviors and seeking effective treatments can significantly reduce the risk of atrial fibrillation and its associated complications.
In light of the diverse risk factors contributing to atrial fibrillation, a tailored, multidisciplinary approach is essential for optimal care. Dr. Nikhil Warrier, a cardiac electrophysiologist, highlighted that, considering each patient's unique underlying risk factors, conversations focused on addressing primary triggers like alcohol intake in one case and encouraging exercise in another may be beneficial. Dr. Yehoshua Levine, a cardiologist, agreed, emphasizing that the optimal management of atrial fibrillation necessitates the consideration of various clinical, demographic, and socioeconomic factors when determining the most appropriate treatment approach.
- Atrial fibrillation, a prevalent arrhythmia, raises the risk of strokes significantly.
- The management of atrial fibrillation requires a comprehensive approach, extending beyond medication.
- Non-modifiable risk factors for atrial fibrillation include genetics, sex, and age.
- Blood thinners or anticoagulants can help reduce the risk of stroke in individuals with atrial fibrillation.
- Lifestyle changes and medications can effectively manage atrial fibrillation, despite being a complex disease with numerous risk factors.
- Obesity, physical inactivity, smoking, and excessive alcohol consumption raise the risk of atrial fibrillation and its severity.
- Proper management of comorbidities like hypertension, diabetes, coronary artery disease, and other cardiovascular conditions can help lower the risk of atrial fibrillation.
- Lifestyle changes, medications, and invasive procedures like catheter ablation can restore a normal heart rhythm for those with atrial fibrillation.
- Other modifiable risk factors for atrial fibrillation include elevated blood pressure, unhealthy sleep patterns, poor mental health, high alcohol intake, unhealthy diets, and smoking.
- A tailored, multidisciplinary approach is crucial for optimal care of atrial fibrillation, considering each patient's unique risk factors and underlying conditions.