Long-Term Impact of Tramadol on the Brain: Unraveling Potential Permanent Harm
Venture into the complex world of Tramadol and brain function, as we examine the potential long-term consequences of this opioid medication on the human brain. This exploration delves into whether Tramadol can cause permanent brain damage and offers crucial insights into the safe use of this drug.
Get a grip on Tramadol's brain-bending tricks
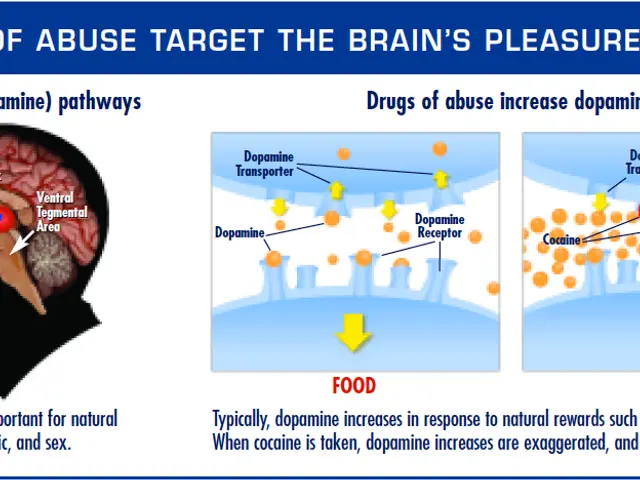
To fully understand Tramadol's long-term impact on the brain, we must first comprehend its unique working mechanism. Tramadol operates with a dual-action that sets it apart from other opioids: it binds to mu-opioid receptors in the brain, just like other opioids, but it also obstructs the reabsorption of two essential neurotransmitters – serotonin and norepinephrine – that govern mood regulation and pain perception.
The fusion of these two actions results in effective pain relief, but it also adds complexity when contemplating the drug's effect on brain chemistry. In the short term, Tramadol can incite various responses on the central nervous system:
- Pain relief
- Mood elevation
- Sedation
- Potential cognitive impairment
One of Tramadol's major worries is its potential for addiction and dependence, much like other opioids. Tramadol can create a sense of euphoria and general well-being, which could lead to improper use and addiction. This danger is particularly relevant when considering long-term effects on brain function, as prolonged exposure to the drug might distort brain chemistry and structure.
Exploring the Outer Limits: Long-Term Effects on Brain Function
While the short-term impacts of Tramadol are well-documented, the long-term influence on brain function remains an ongoing research topic. However, several studies and clinical observations have sparked concerns:
- Cognitive Deterioration and Memory Woes: Some users report problems with concentration, memory, and overall cognitive performance after Tramadol use over an extended period. These difficulties can persist even after discontinuing the drug in some instances.
- Mood Makeovers: Long-term Tramadol use may result in alterations of mood regulation. This could manifest as enhanced irritability, anxiety, or even depression. The association between Tramadol and depression is especially significant and will be further scrutinized in this context.
- Neuoplasticity and Brain Structure Twists: Emerging research suggests that persistent opioid use, including Tramadol, may induce changes in brain structure and functionality. These modifications can affect regions of the brain responsible for decision-making, impulse control, and emotional regulation.
It's essential to note that the severity and longevity of these effects might vary significantly among individuals, relying upon factors like dose duration, usage frequency, and individual physiology.
Can Tramadol cause permanent brain damage?
The question of whether Tramadol can cause permanent brain damage is still debatable and not yet conclusively answered by current research. While evidence indicates potential long-term effects on brain function, the extent to which these alterations are reversible or irreversible is yet to be determined.
The current research suggests that while Tramadol usage may lead to changes in brain function and structure, many of these changes can be reversed with appropriate treatment and cessation of the drug. However, the possibility of long-lasting or permanent effects cannot be entirely ruled out, especially in cases of prolonged, high-dose use or abuse.
Factors that may increase the risk of brain damage include:
- Duration and dose of Tramadol usage
- Individual genetic factors
- Pre-existing mental health conditions
- Simultaneous use of other substances
The reversibility of potential brain changes significantly depends on the specific case and the specific brain regions influenced. Some users may experience a full recovery of cognitive function following Tramadol cessation, while others may grapple with persistent consequences that necessitate further treatment and support.
Dancing with Depression: Tramadol's Link to Depression
One of the most critical concerns with Tramadol's long-term effects is its link to depression. This connection is particularly intricate due to Tramadol's dual effect on both opioid receptors and neurotransmitter systems.
Tramadol modifies neurotransmitters linked to mood, most notably serotonin and norepinephrine. While this impact contributes to its pain-alleviating effects, it also influences mood regulation. Some studies suggest that Tramadol might have antidepressant-like effects in some individuals, provoking its off-label use for depression in certain cases.
However, paradoxically, Tramadol use has been associated with an increased risk of developing depression, particularly with long-term use. This raises the question: Is Tramadol an antidepressant, or does it cause depression?
The solution lies likely in the complex interplay between pain, mood, and medication effects. Chronic pain itself is a risk factor for depression, making it difficult to discern between pain-related depression and possible drug-induced mood changes. Furthermore, the development of tolerance and dependence on Tramadol can induce withdrawal symptoms when the medication is not accessible, which may mimic or exacerbate depressive symptoms.
Countermeasures: Using Tramadol with Caution and Alternatives
Given the potential risks associated with long-term Tramadol usage, it's crucial to approach its use with prudence and under close medical supervision. Here are some guidelines for responsible Tramadol usage:
- Strictly adhere to prescribed dosages
- Regularly communicate with healthcare providers regarding the medication's efficacy and any side effects
- Be aware of potential interactions with other medications or substances
- Never abruptly stop using Tramadol without medical guidance, as this may lead to severe withdrawal symptoms
For those concerned about long-term effects of Tramadol or seeking alternatives, various pain management strategies are available:
- Non-opioid pain medications (e.g., NSAIDs, acetaminophen)
- Physical therapy and exercise
- Cognitive-behavioral therapy for pain management
- Alternative therapies such as acupuncture or massage
- Exploring other medications for specific symptoms such as sleep disorders or anxiety
It's essential to consult with a healthcare professional if you have concerns about Tramadol usage or experience side effects. They can help assess your individual situation and suggest appropriate alternatives or adjustments to your treatment plan.
In conclusion, while Tramadol is an effective pain management tool, its long-term use carries potential risks to brain health that should not be disregarded. Current research indicates that while some effects on brain function might occur with prolonged use, many of these changes can be reversed with proper treatment and Tramadol cessation. However, the possibility of more long-lasting impacts, particularly in instances of misuse or high-dose, long-term use, underscores the importance of informed decision-making and close medical supervision.
As our understanding of Tramadol's long-term effects continues to develop, future research will most likely provide more definitive answers about its impact on brain health. In the meantime, patients and healthcare providers must weigh the benefits of pain relief against the potential risks, taking individual factors and alternative pain management strategies into account.
It's worth noting that the concerns surrounding Tramadol are not exclusive to this medication. Analogous questions have been posed about other pain medications and psychoactive substances. For instance, research has looked into the long-term effects of Percocet and questioned whether hydrocodone causes depression. These ongoing investigations underscore the complexity of handling chronic pain while minimizing long-term health risks.
Ultimately, the key to responsible and effective pain management lies in open communication with healthcare providers, persistent monitoring of medication effects, and a readiness to explore diverse treatment approaches. By staying informed and proactive, patients can strive towards achieving pain relief while minimizing the risk of long-term adverse effects on brain health.
- The dual-action mechanism of Tramadol that affects both opioid receptors and neurotransmitters could lead to long-term anxiety due to alterations in mood regulation.
- Managing sleep issues might be complicated when using Tramadol for an extended period, as its effect on neurotransmitters could impact sleep patterns.
- In the exploration of alternatives for long-term pain management, various mental-health-focused therapies-and-treatments, such as cognitive-behavioral therapy, can help address potential mental health concerns associated with Tramadol use.
- To preserve overall health-and-wellness, it's crucial to consider the long-term mental health implications of substances like Tramadol and take preventative measures, such as exploring nutritional supplements or lifestyle modifications, to support brain function and recovery.
- As part of a comprehensive pain management strategy, healthcare providers may recommend psychotherapy and lifestyle interventions as adjunctive therapies to address sleep, anxiety, and other symptoms associated with prolonged Tramadol use.