Narcolepsy and Schizophrenia: Are These Disorders Secretly Connected?
Narcolepsy and schizophrenia can sometimes be mistaken for each other due to overlapping symptoms. Both conditions may involve hallucinations and disrupted sleep patterns, leading to potential misdiagnosis. Yet recent studies suggest a possible link between the two, raising questions about their relationship.
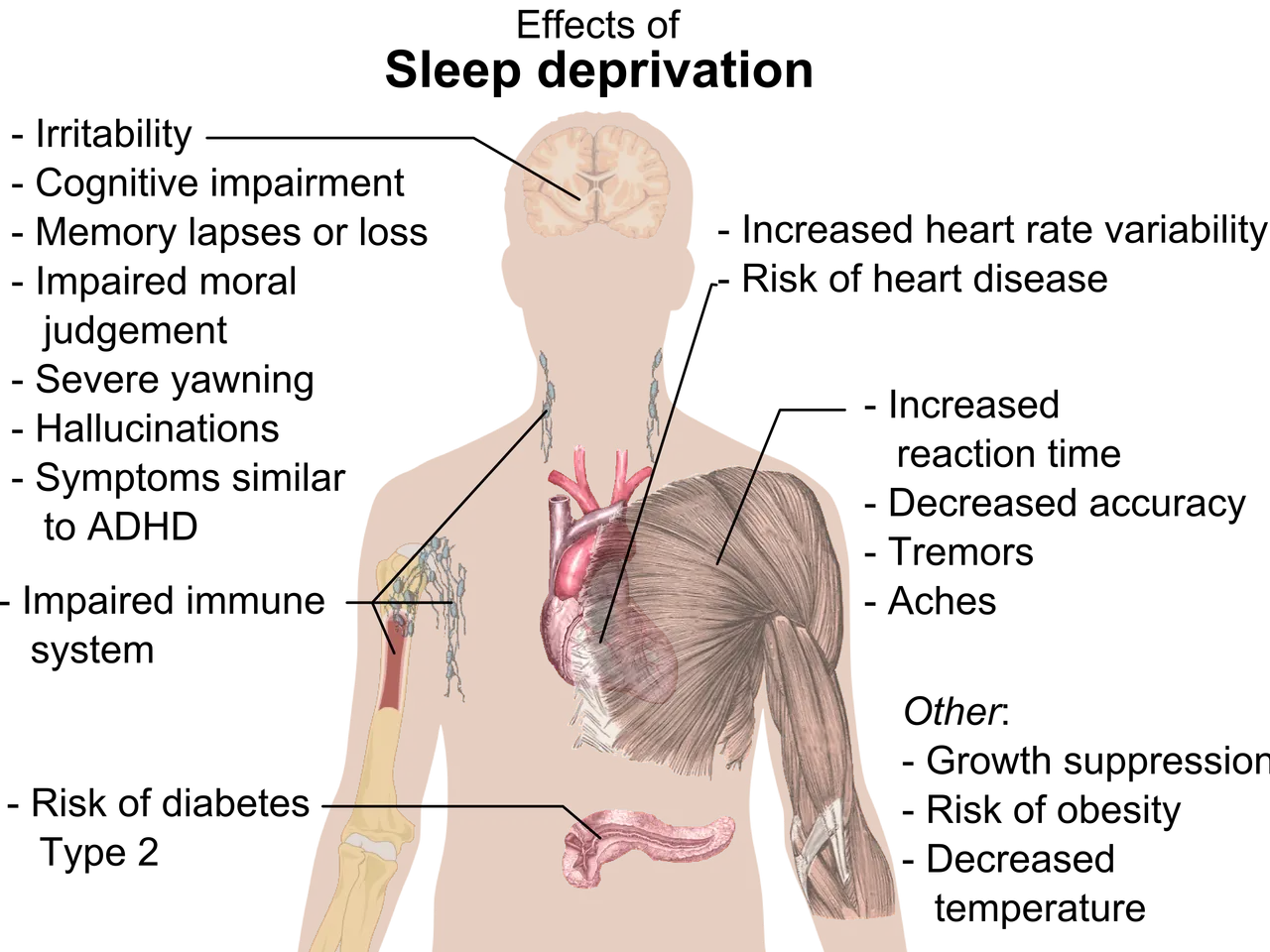
Narcolepsy is a neurological disorder that disrupts sleep-wake cycles. It causes excessive daytime sleepiness, sudden muscle weakness (cataplexy), sleep paralysis, and insomnia. Schizophrenia, on the other hand, is a brain disorder marked by hallucinations, delusions, disorganised speech, and impaired thinking.
Despite their differences, the two conditions share some symptoms, such as hallucinations. In narcolepsy, these often occur during transitions between sleep and wakefulness, while in schizophrenia, they happen while fully awake. The timing and nature of these hallucinations can help doctors distinguish between the two. Research has explored whether narcolepsy increases the risk of developing schizophrenia. A 2020 study found that people with narcolepsy were four times more likely to develop a psychotic disorder. A 2025 study further supported this, showing a higher prevalence of schizophrenia among those with narcolepsy, hinting at a possible two-way influence. Currently, no direct biological link has been confirmed between the two conditions. However, treatments for narcolepsy, such as stimulants like methylphenidate, carry warnings. These medications can worsen psychotic symptoms in patients with schizophrenia or a history of it.
The overlap in symptoms between narcolepsy and schizophrenia can make diagnosis challenging. Studies now suggest a potential connection, with narcolepsy possibly raising the risk of schizophrenia. Further research is needed to clarify the relationship and improve diagnostic accuracy for both conditions.