Navigating the Intersection of Workers' Compensation and Medicare: Crucial Facts to Consider
Let's Get the Lowdown on Workers' Comp and Medicare
Navigating the waters of workers' compensation and Medicare can be tricky, but here's a simplified guide to help you avoid potential pitfalls.
'Workers' comp' is an insurance policy for employees who've suffered job-related injuries or illnesses. The Office of Workers' Compensation Programs under the Department of Labor administers this benefit for federal employees and certain other entities.
If you're currently on Medicare or soon will be, it's vital to understand how workers' compensation might impact your Medicare coverage. This can prevent any complications with medical costs for work-related injuries or illnesses.
How does a workers' comp settlement impact Medicare?
Under Medicare's secondary payer policy, workers' compensation must cover any treatment for a work-related injury first. If immediate medical expenses arise before the settlement, Medicare may pay the bills initially and initiate a recovery process managed by the Benefits Coordination & Recovery Center (BCRC).
To avoid a recovery process, the Centers for Medicare & Medicaid Services (CMS) often monitors the amount a person receives from workers' compensation for injury-related medical care. In some cases, Medicare may ask for the establishment of a workers' compensation Medicare set-aside arrangement (WCMSA) for these funds. Medicare won't cover any care until the money in the WCMSA is used up.
What settlements need to be reported to Medicare?
Workers' compensation must submit a total payment obligation to the claimant (TPOC) to CMS. This includes the total amount owed to the person or on their behalf.
You need to submit a TPOC:
- If you're already enrolled in Medicare, and the settlement is $25,000 or more.
- If you're not yet enrolled in Medicare but will qualify for the program within 30 months of the settlement date, and the settlement amount is $250,000 or more.
Additionally, you must report if you file a liability or no-fault insurance claim.
FAQs
- Contact Medicare by phone at 800-MEDICARE (800-633-4227, TTY 877-486-2048) or through a live chat on Medicare.gov during certain hours. For questions about the Medicare recovery process, you can contact the BCRC at 855-798-2627 (TTY 855-797-2627).
- A Medicare set-aside is voluntary but mandatory if the workers' compensation settlement is over $25,000 or $250,000 in certain cases.
- Misusing the money in a Medicare set-aside arrangement can lead to claim denials and reimbursement obligations.
For more resources on medical insurance, visit our hub.
Starting April 4, 2025, every full and final workers' compensation settlement involving a Medicare beneficiary must be reported to CMS. The settlement must be reported through the Medicare Secondary Payer (MSP) Section 111 reporting process, providing details such as the total settlement amount, the Medicare Set-Aside allocation (if applicable), and the settlement funding mechanism (e.g., lump sum or structured annuity).
By ensuring proper reporting, Medicare will be able to monitor the use of settlement funds for future medical treatment related to the injury. Failure to report properly can lead to denial of Medicare benefits for treatment related to the injury, and potentially result in civil penalties or litigation.
TakeawayIf you're on Medicare or soon will be, understand the impact of workers' compensation on your Medicare coverage. Ensure that workers' compensation settlements are reported to Medicare through the Section 111 process to protect your Medicare coverage for future medical expenses related to your injury.
- The navigation of healthsystems involving workers' compensation and Medicare requires careful understanding to prevent conflicts with medical costs for work-related injuries or illnesses.
- Under the secondary payer policy of Medicare, workers' compensation must cover any treatment for work-related injuries before Medicare steps in.
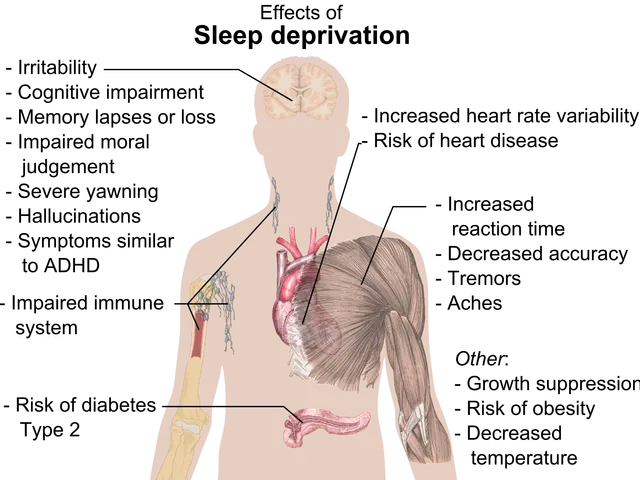
- Chronic diseases, particularly chronic kidney disease, can be a component of medical-conditions requiring long-term treatments that might be covered by workers' comp settlements.
- In the context of health-and-wellness, fitness-and-exercise, and nutrition play crucial roles in managing chronic-diseases and overall well-being, which can be affected by work-related injuries or illnesses.
- Science plays a significant role in understanding the implications of chronic-kidney-disease, as well as the impact of workers' compensation settlements on Medicare coverage, aiming to develop more effective strategies and policies for both systems.