Orgasms and potential resulting headaches: An examination
Sex-induced headaches, also known as coital cephalalgia or headache associated with sexual activity (HAS), are a lesser-known yet common type of headache that can occur during or after sexual activity [1].
Causes of HAS
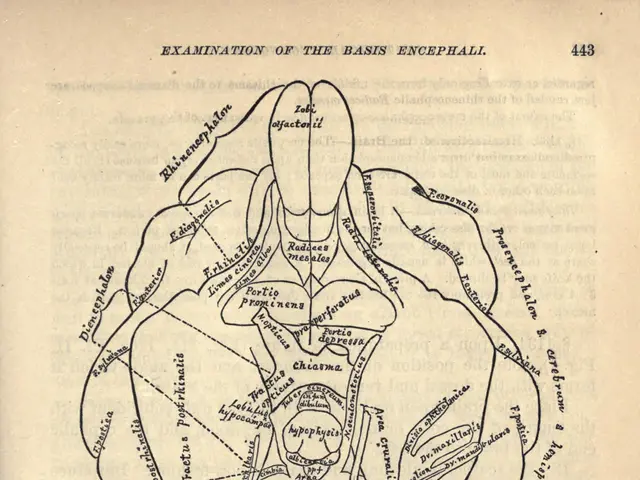
The exact cause of HAS is not yet fully understood, but it is believed to be related to vascular changes in the brain during sexual activity. These changes can include increased blood pressure and muscle tension [1]. For individuals with a history of migraines, sexual activity can act as a trigger due to the overlap in the vascular and neurological pathways involved in both conditions [1].
Hormonal fluctuations, particularly in women, may also influence migraine susceptibility and potentially exacerbate sex-induced headaches [2]. Common migraine triggers, such as physical exertion or stress, may also contribute to HAS.
Treatments for HAS
Preventive treatment for HAS may include beta-blockers like propranolol, which have shown effectiveness in preventing headache chronicity and reducing sensitivity [1][3]. The use of indomethacin, a nonsteroidal anti-inflammatory drug (NSAID), is sometimes prescribed 30-60 minutes before sexual activity to prevent headaches [3].
Identifying and avoiding individual migraine triggers through headache diaries can help manage the risk of HAS [2]. General supportive measures include relaxation techniques and avoiding excessive physical exertion that could trigger headaches.
In cases where secondary causes are suspected (rare but serious causes like aneurysms), medical evaluation is essential to rule out other conditions. For people with a history of migraines experiencing sex-induced headaches, consultation with a neurologist is recommended. They may tailor treatment based on migraine history and headache characteristics.
When to Seek Medical Attention
If you experience a severe sexual headache, seek immediate medical attention to rule out serious causes. When blood pressure increases during sex, the force can be enough to make a brain aneurysm bulge rupture [1].
It's important to note that while over-the-counter pain relievers like acetaminophen (Tylenol®) or ibuprofen (Advil®) can be used to treat sex headaches if no serious cause is found, they should not replace professional medical advice.
In summary, sex-induced headaches often involve vascular and neurological mechanisms similar to migraines, and treatments such as beta-blockers (e.g., propranolol) and NSAIDs (e.g., indomethacin) are commonly used preventive options [1][3]. Hormonal factors can influence migraine susceptibility, which may exacerbate this condition in some individuals [2].
References: [1] Mayo Clinic. (2021). Sex-induced headaches. Retrieved from https://www.mayoclinic.org/diseases-conditions/sex-induced-headaches/symptoms-causes/syc-20373462 [2] Headache On the Net. (2021). Coital cephalalgia. Retrieved from https://www.headache-on-net.org/professionals/classification-diagnostic-criteria/coital-cephalalgia [3] National Headache Foundation. (2021). Sexual headaches. Retrieved from https://www.headaches.org/2021/04/sexual-headaches/
Mental health, just like physical health, plays a crucial role in overall well-being and the management of sex-induced headaches. Stress, a common migraine trigger, can contribute to HAS and is closely related to mental health [2].
Sexual health is another aspect to consider. Understanding correlations between sexual activity and headaches, such as coital cephalalgia, contributes to the broader field of health-and-wellness.
In the history of medical research, advancements in both neurology and vascular science have helped illuminate the vascular mechanisms underlying sex-induced headaches, aiding in the development of targeted treatments [1].