Predictive Approaches in Immunotherapy: Scientists Discover Methods to Forecast Treatment Results
Every year, scientists are making strides in the fight against cancer with the development of new treatment options. One of the most promising is immunotherapy, which harnesses the body's immune system to combat the disease.
Sadly, immunotherapy isn't the magic bullet for every single cancer patient. Researchers have been scrambling to find answers as to what makes immunotherapy effective for some but not for others. Now, scientists from Johns Hopkins University may have found a clue: a specific subset of mutations in cancer tumors that suggests how receptive the tumor will be to immunotherapy.
These researchers believe their findings can help doctors make better decisions about who to administer immunotherapy to and what outcomes to expect. Their research, recently published in the journal Nature Medicine, is a game-changer in the world of cancer treatment.
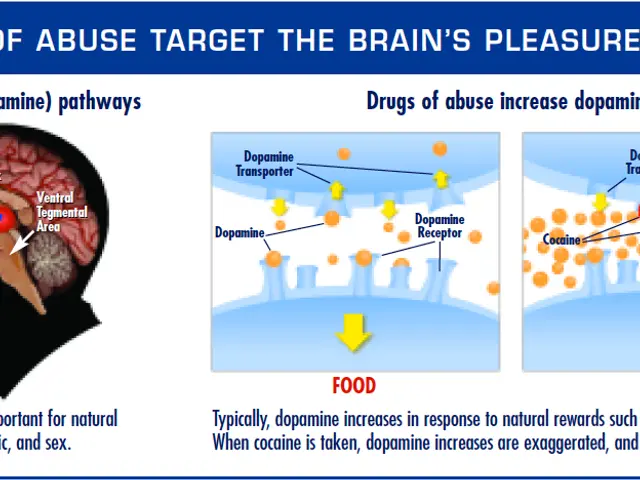
So, what exactly is immunotherapy? Good question. It's a treatment that enhances the body's ability to find and destroy cancer cells by boosting the immune system. Immunotherapy comes in various forms, including checkpoint inhibitors, CAR T-cell therapy, and vaccines.
Currently, immunotherapy is an option for breast cancer, melanoma, leukemia, and non-small cell lung cancer. Scientists are also investigating its potential use in treating other forms of cancer, such as prostate cancer, brain cancer, and ovarian cancer.
According to the study, doctors use a specific measure called the tumor mutation burden (TMB) to determine if a tumor will respond well to immunotherapy. This refers to the total number of changes in the cancer cells' genetic material. A high number of mutations means the cancer cells are more distinct from normal cells, making them more visible to the immune system and therefore more likely to respond to immunotherapy.
However, the Johns Hopkins researchers went a step further. They discovered a specific subset of mutations within the overall TMB, which they named "persistent mutations." These mutations are less likely to disappear as the cancer evolves, keeping the tumor visible to the immune system and boosting the chances of a positive response to immunotherapy.
"Persistent mutations allow the cancer tumor to remain visible to the immune system, facilitating a better response to immunotherapy," said Dr. Valsamo Anagnostou, a senior author of the study and an associate professor of oncology at Johns Hopkins. "The number of persistent mutations can better identify tumors that are more likely to respond to immune checkpoint blockade compared to the overall TMB."
The researchers believe the new findings can help doctors more accurately select who should receive immunotherapy and predict the outcomes for those patients. It's a major step towards personalized medicine for cancer treatments.
Of course, there's still a lot to learn about cancer and immunotherapy. But with groundbreaking research like this, we're one step closer to vanquishing this scary disease once and for all.
- In the realm of medical-conditions like cancer, scientists are increasingly exploring therapies-and-treatments such as immunotherapy to combat the disease.
- Immunotherapy is a health-and-wellness approach that enhances the body's immune system, enabling it to locate and destroy cancer cells more effectively.
- The study by scientists from Johns Hopkins University has identified a specific subset of mutations, termed "persistent mutations," within the tumor mutation burden (TMB), which could potentially assist doctors in making informed decisions about immunotherapy treatments.
- This discovery could lead to a more personalized system of administering immunotherapy, where the number of persistent mutations can help predict which cancer patients are more likely to respond positively to immune checkpoint blockade treatments.