Psoriatic arthritis in action: Understanding its features, identification methods, remedies, and additional details
In the realm of chronic illnesses, psoriatic arthritis (PsA) is a condition that often coexists with psoriasis, a skin condition marked by scaly, irritated plaques. This article aims to shed light on the common symptoms, triggers, and treatment options for active PsA.
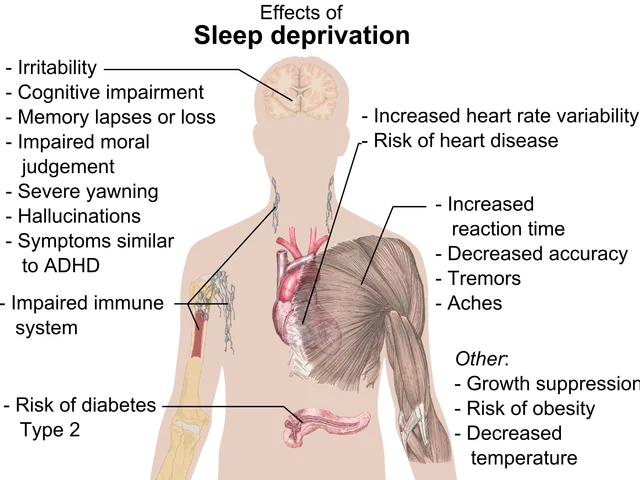
Active PsA often presents with a range of symptoms, including joint pain, swelling, and stiffness, particularly in the knees, hands, feet, and fingers or toes. The inflammation can sometimes cause the fingers and toes to appear swollen like a "sausage" - a condition known as dactylitis. Enthesitis, or inflammation where tendons or ligaments attach to bone, can lead to localized pain and stiffness. Other symptoms may include fatigue, psoriatic skin and nail changes, eye inflammation, and lower back pain from spine involvement (spondylitis) [1][3][4][5].
Triggers for PsA flare-ups are often a combination of genetic and environmental factors. Stress, infections, trauma, or other inflammatory triggers can precipitate or worsen flares, although exact triggers vary by individual [2][4].
Treatment for active PsA is multi-faceted, aiming to reduce inflammation, relieve symptoms, prevent joint damage, and improve quality of life. This can involve medications such as nonsteroidal anti-inflammatory drugs (NSAIDs) for pain and swelling, conventional disease-modifying antirheumatic drugs (DMARDs) like methotrexate, and biologic agents targeting immune pathways (e.g., TNF inhibitors, IL-17 or IL-23 inhibitors) [5].
In addition to medication, lifestyle changes and supportive approaches can play a significant role in managing symptoms. Stress reduction, regular exercise, and dietary supplements like turmeric (curcumin) with anti-inflammatory properties may help [2]. Early diagnosis by a rheumatologist and ongoing monitoring are crucial to tailor treatment and avoid permanent joint damage [1][4].
It's essential to remember that everyone's experience with PsA is unique. Symptoms may include swollen joints, especially in the hands and feet, and skin symptoms such as plaques or scaly spots [1][3][4][5]. Physical therapy and occupational therapy may be recommended to improve mobility and help manage pain.
For those experiencing PsA symptoms, it's crucial to seek medical advice. A person should contact a doctor if their PsA symptoms do not improve with treatment, if the treatment causes unpleasant side effects, if they develop symptoms of psoriasis for the first time, if they develop joint pain, or if they have questions about treatment options or symptom management [1]. A rheumatologist can work with a person to develop a personalized treatment plan for PsA [1].
In conclusion, active PsA is a complex condition driven by immune-mediated inflammation. Flares can be triggered by various factors, and treatment combines medication, lifestyle changes, and specialist care to control disease activity and prevent progression. Early treatment and identifying triggers can significantly improve outcomes for those living with PsA.
References:
[1] National Psoriasis Foundation. (2021). Psoriatic Arthritis. Retrieved from https://www.psoriasis.org/about-psoriasis/psoriatic-arthritis
[2] Mayo Clinic. (2021). Psoriatic arthritis. Retrieved from https://www.mayoclinic.org/diseases-conditions/psoriatic-arthritis/symptoms-causes/syc-20368574
[3] American College of Rheumatology. (2019). 2018 Update of the ACR/EULAR Recommendations for the Classification and Treatment of Psoriatic Arthritis. Arthritis Care & Research, 71(1), 5-22. doi: 10.1002/acr.23967
[4] National Institute of Arthritis and Musculoskeletal and Skin Diseases. (2021). Psoriatic Arthritis. Retrieved from https://www.niams.nih.gov/health-topics/psoriatic-arthritis
[5] European League Against Rheumatism. (2020). EULAR recommendations for the management of psoriatic arthritis with biologic disease-modifying antirheumatic drugs. Annals of the Rheumatic Diseases, 79(2), 215-226. doi: 10.1136/annrheumdis-2019-215273
- Seekers of information about Psoriatic Arthritis (PsA) should understand that it commonly coexists with psoriasis, a skin condition characterized by scaly, irritated plaques.
- Persons diagnosed with PsA may experience a range of symptoms, such as joint pain, swelling, and stiffness, particularly in the knees, hands, feet, and fingers or toes.
- Switchers from traditional treatments to biologic agents may find relief, as these target immune pathways related to PsA.
- Despite the chronic nature of PsA, science continues to explore new treatments for this condition and others like chronic kidney disease and various health-and-wellness issues.
- A naive approach to PsA management might overlook the importance of lifestyle changes and supportive approaches like stress reduction, regular exercise, and dietary supplements.
- In addition to medications, rheumatologists may recommend physical therapy or occupational therapy for those with PsA to improve mobility and help manage pain.
- Those with chronic diseases like PsA, psoriasis, and other skin conditions should prioritize fitness-and-exercise and maintain a healthy diet for overall health improvement.
- Medical-conditions such as PsA can present unique symptoms for each individual, making it essential for persona to discuss their experiences and questions about treatment options or symptom management with a rheumatologist.