Science is transforming our concepts of life and demise
In a thought-provoking interview at the Morgan Library and Museum in New York, intensive care physician Dr. Sam Parnia discussed the latest developments in resuscitation medicine with Steve Paulson as part of the series "Spirituality in the Age of Science."
Dr. Parnia, one of the world's leading experts in resuscitation medicine, is based at the New York University School of Medicine. He believes that recent advancements in the field will not only save more lives but also shed light on deep questions about the nature of death.
One groundbreaking study, led by Dr. Nenad Sestan from Yale University, made headlines in 2019. The researchers were able to revive the brains of decapitated pigs, showing full biological and metabolic activity. These findings, published in Nature, suggest that the technology to revive human brains may already exist.
However, the scientists involved in the study expressed concerns about the implications of their findings and decided to downplay them. Dr. Parnia, on the other hand, sees this as an opportunity to challenge society's understanding of death as a rapid degradation process. Instead, he proposes that there is a long "gray zone" in which cells enter a hibernation state.
This idea is not new. In the 1950s and 60s, people with catastrophic brain injuries were kept alive on life support machines, leading to the legal notion that a person can be declared dead if their brain has died while on a ventilator. However, Dr. Parnia suggests a new approach to resuscitation that involves connecting people who die to catheters to distribute oxygenated blood, nutrients, and a cocktail of drugs to preserve the brain.
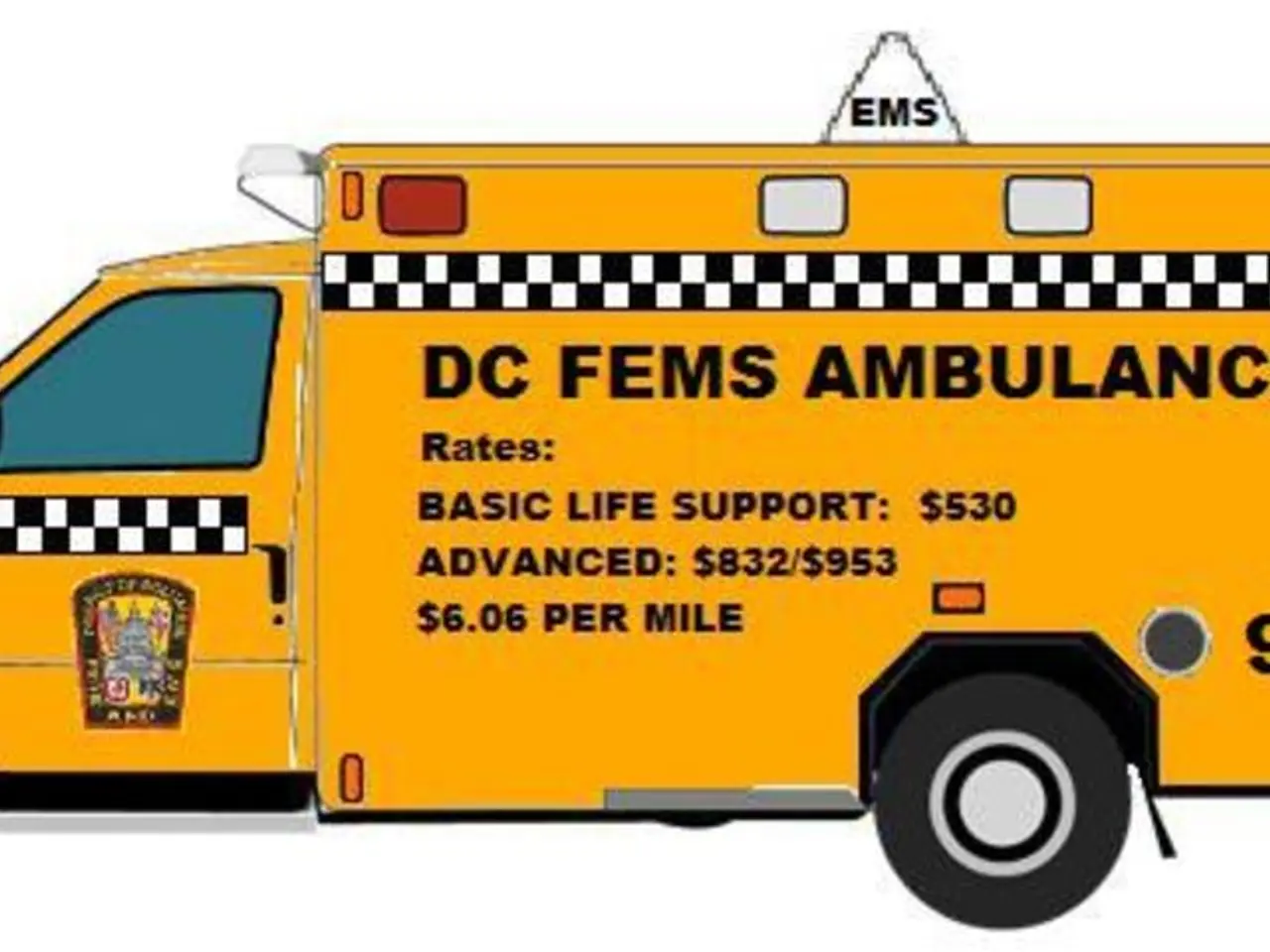
These advancements in resuscitation medicine are gradually enabling the revival of patients hours after clinical death. This transformation in end-of-life and emergency medical care is due to progress in prolonged resuscitation techniques, diagnostic assessment, trauma care, and supportive pharmacology.
For example, evolving brain resuscitation techniques coupled with multimodal neuroprognostication—using multiple diagnostic tools to more accurately assess neurological recovery potential—are helping clinicians decide when and how to continue life support efforts beyond traditional time limits. Timely interventions such as early transfusion protocols and damage control resuscitation have significantly extended survival windows, sometimes enabling revival hours after initially deemed fatal injury or arrest.
The integration of artificial intelligence and advanced simulation training in pre-hospital and critical care settings further enhances rapid, precise resuscitation efforts during those critical windows. Pharmacological advances, such as modulation of sirtuin pathways, hint at future molecular targets that might protect tissues during ischemic periods and assist recovery post-arrest.
The upcoming global resuscitation science conferences, such as WRC 2025 and TICEM ASM, underscore a growing international collaboration focused on advancing trauma, toxicology, resuscitation science, and pre-hospital care. These forums are tracking innovations that promise to push the boundaries of what is medically reversible in cardiac arrest and critical illness.
The impact of these advancements on future end-of-life medical care may be profound. They could redefine criteria for clinical death and expand the time frames in which resuscitative efforts are ethically and medically justified. This may lead to revised protocols that integrate advanced neuroprognostication, prolonged organ support technologies, and precision pharmacology to maximize patient survival with meaningful neurological recovery.
Moreover, these advancements may influence policies on organ donation, post-arrest care, and decision-making around withdrawal of life support, fostering a shift towards more individualized and optimistic approaches to patients previously considered beyond saving.
In conclusion, recent progress in prolonged resuscitation techniques, diagnostic assessment, trauma care, and supportive pharmacology is gradually enabling the revival of patients hours after clinical death, thus promising to transform the landscape of end-of-life and emergency medical care in the near future.
Science and medical-conditions have intersected in a groundbreaking study, as researchers revived the brains of decapitated pigs, showcasing full biological and metabolic activity. This discovery, published in Nature, points towards the possibility of reviving human brains, raising questions about the nature of death and challenging societal beliefs (science, medical-conditions).
As a part of the series "Spirituality in the Age of Science," Dr. Parnia, a leading expert in resuscitation medicine, discussed the advancements in the field and their implications on end-of-life medical care (science, series).
In health-and-wellness and fitness-and-exercise discussions, these advancements may lead to revised protocols and expanded time frames for resuscitative efforts, which can influence policies on organ donation, post-arrest care, and life support withdrawal (health-and-wellness, fitness-and-exercise).