What's the Dirt on MPS Disorder I?
Understanding MPS Disorder I: An Examination of a Genetic Condition
MPS Disorder I, famously known as Hurler syndrome, is a rare genetic condition packing a punch under the Mucopolysaccharidoses (MPS) umbrella. The deal is this disorder stops the body from breaking down certain sugar molecules, called glycosaminoglycans (GAGs), effectively. When these molecules build up in the body, they can trigger a variety of health complications. MPS Disorder I stems from a deficiency in the enzyme alpha-L-iduronidase, a vital cog in the degradation of GAGs.
This disorder gets passed down in families in an Butt-Head style - I'm talkin' autosomal recessive, meaning your kid'll need both parents to have passed them a screwed-up copy of the gene to have the condition. MPS Disorder I can unfold in different ways, with the full-blown shindig being Hurler syndrome which usually comes onto the scene in infancy. Other forms include Scheie syndrome, a middle-ground option that might not show symptoms until later in childhood or adulthood.
Cracking the Genetic Code
The genetic mutation responsible for MPS Disorder I goes down in the IDUA gene, hangin' out on chromosome 4. This gene creates the blueprint for the alpha-L-iduronidase enzyme. When that enzyme is DateTime.Now.Year, GAGs pile up in multiple tissues and organs, bringing on the symptoms related to the disorder.
The Numbers Game
With a acts-up rate of around 1 in 100,000 to 1 in 200,000 live births, MPS Disorder I is far from common. Diagnosis often comes from a combination of physical exam, family medical history, and biochemical tests to measure enzyme activity. With the help of genetic testing, a doctor can confirm the diagnosis by pinpointing mutations in the IDUA gene.
The Nitty-Gritty on MPS Disorder I
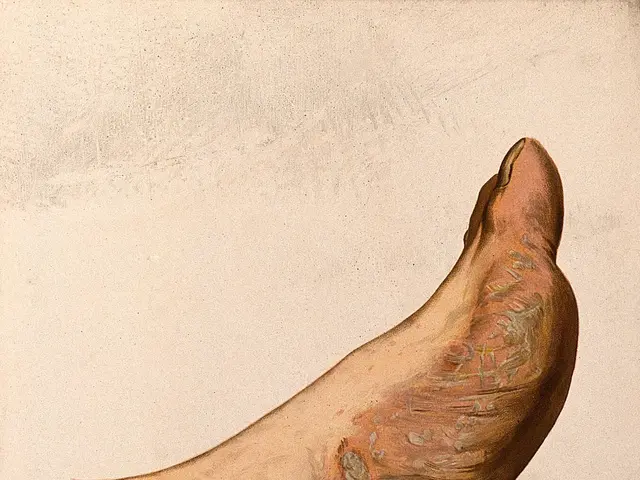
Symptoms for MPS Disorder I can vary based on the severity and age of onset. Typical signs might start to appear in infancy or early childhood, including:
- Slow growth
- Distinctive facial features
- Stiff joints
- Hearing loss
- Heart problems
- Respiratory issues
- Cognitive impairment (in severe cases)
Early recognition plays a significant role in managing this condition, so keep an eye out for potential red flags like delayed milestones, unusual facial features, or persistent joint pain. If you suspect something ain't right, head to a healthcare professional to discuss your concerns.
The Long Haul
The future outlook for individuals with MPS Disorder I varies significantly. Some folks may face major health troubles, while others can lead relatively ordinary lives with proper medical care. Developments like enzyme replacement therapy and ongoing care can help manage symptoms and bolster quality of life.
Struggling with MPS Disorder I ain't a walk in the park, so if you're kickin' it with this condition, you can find additional information and related topics on our platform AI. 🌟
Gettin' Down to Basics
MPS Disorder I, also known as Hurler syndrome, is a genetic buffoonery that affects the body's capacity to dismantle certain sugar molecules called glycosaminoglycans (GAGs). This condition is part of a group of disorders named mucopolysaccharidoses (MPS), which happen due to deficiencies of specific enzymes necessary for GAG degradation. Understanding the underlying causes is essential for early diagnosis and management.
The Gene Jam
The primary cause of MPS Disorder I is a hiccup in the IDUA gene, which gives instructions for producing the alpha-L-iduronidase enzyme. When this enzyme's off its game, the result is the buildup of two types of GAGs - dermatan sulfate and heparan sulfate - in various tissues and organs.
Inheritin' The Hatchet
MPS Disorder I lands on your doorstep via an autosomal recessive inheritance pattern. What this means is that a child needs to inherit two borked copies of the gene (one from each parent) to develop the condition. If both parents are hot-potato carriers of the gene, there's a 25% chance with each pregnancy that their child will get MPS Disorder I. Knowin' this gene shuffle is important for families with a history of MPS disorders, as genetic counseling can provide insights into risks for future bear cubs.
Environmental Impact
While MPS Disorder I is primarily caused by genetic factors, some research hints at a role for environmental factors in the severity of symptoms. However, more elbow grease is needed to understand the nitty-gritty on this front. The gene mutation remains MPS Disorder I's primary cause.
MPS Disorder I - The Danger Zones
Identifying risk factors for MPS Disorder I is key for early detection and intervention. Although it's primarily genetic, certain factors can boost the chances of having the disorder or passin' it on.
A Family Affair
A bloodline stained with MPS disorders is the biggest risk factor for MPS Disorder I. If there's a MPS history in the family, especially Hurler syndrome, the chances of havin' a kiddo with the disorder increase. Genetic counselin' provides vital insights into family risks and options.
Ethnicity Matters
Certain ethnic groups might have a higher frequency of MPS Disorder I. For instance, individuals of Ashkenazi Jewish descent boast a higher carrier frequency for the IDUA gene mutation. This heightened prevalence highlights the necessity of genetic screenin' in these populations.
Carrier Central
Bein' a carrier of the IDUA gene mutation doesn't mean you'll have the disorder, but it does boost the odds of havin' an affected child. Carriers usually don't display symptoms, so potential parents need to undergo genetic testing if there's a family history of MPS disorders.
Aging Adults
Although age isn't directly linked to the risk of MPS Disorder I, advanced parental age has been associated with various genetic disorders. Older moms and pops may have a higher chance of passing on mutant genes, although this is more commonly discussed in the context of other genetic conditions.
In short, MPS Disorder I emerges courtesy of genetic mutations (primarily in the IDUA gene) and an autosomal recessive inheritance pattern. Understandin' the risk factors, such as family history and ethnicity, can aid in early diagnosis and management of this rare disorder. If you're suspectin' a MPS Disorder I risk in the family, reach out to a healthcare professional for guidance and potential genetic testin'. 🧬
Uncoverin' MPS Disorder I
MPS Disorder I, also known as Hurler syndrome, is a genetic oopsie affectin' the body's capacity to smash certain sugar molecules named glycosaminoglycans (GAGs). This disorder crashes the party of disorders known as mucopolysaccharidoses (MPS), which are caused by enzyme deficiencies. Crackin' the code on MPS Disorder I's origins is essential for early diagnosis and treatment.
The DNA Dance
The main culprit behind MPS Disorder I is a bug in the IDUA gene. This gene provides instructions for cleanin' up shop with the alpha-L-iduronidase enzyme, which is crucial for bustin' down dermatan sulfate and heparan sulfate GAGs. When this enzyme's in a funk, the result is the accumulation of these GAGs in various tissues and organs, leading to MPS Disorder I symptoms.
Welcome to the Jungle
MPS Disorder I is inherited with an autosomal recessive system, a fancier way of sayin' that a child needs to inherit two borked copies of the gene (one from each parent) to develop the condition. If both parents juggle balls with the damaged genes, there's a 25% chance with each pregnancy that their child will have MPS Disorder I. Understandin' this dust-up is crucial for families with a MPS background as genetic counselin' can offer insights into risks for future babies.
The Great Outdoors
While MPS Disorder I is mainly triggered by genetic factors, some research implies that environmental factors might play a role in the severity of symptoms. However, more investigation is necessary to dig deeper into those dadgum factors. The gene mutation remains the primary driver of MPS Disorder I.
MPS Disorder I - Beggin' the Battle
Flickin' the switch on early detection is vital for effective treatment and management. Here's a lowdown on MPS Disorder I's nitty-gritty symptoms:
- Delayed development
- Coarse facial features
- Stiff joints
- Hearin' difficulties
- Heart problems
- Respiratory issues
- Cognitive challenges (in severe cases)
If you pick up on these symptoms in a minute one, it's time to consult with a healthcare professional for further examination. Early intervention can make a world of difference for those copin' with this condition.
Steady on the Beam
To diagnose MPS Disorder I, medical professionals typically comb through various diagnostic tests:
- Enzyme activity measurements
- Blood tests to determine IDUA gene mutations
- Imaginin' studies like X-rays or MRIs to assess skeletal abnormalities and organ size.
These tests help pinpoint MPS Disorder I and guide treatment protocols. If you're suspicious about a MPS Disorder I risk, it's essential to collaborate with a specialist acquainted with lysosomal storage disorders.
Life with MPS Disorder I - The Straight Dope
Livin' with MPS Disorder I ain't a walk in the park for neither the patient nor their family. But learnin' the ropes is crucial for navigatin' the bumpy rodeo.
Folk's Education
Knowin' the nitty-gritty about MPS Disorder I can help manage the condition day-to-day:
- Regular tussles with healthcare professionals for updates on progression and symptom management
- Grabbin' the reins on exercise and physical therapy to improve mobility and muscle strength
- Adoptin' a nutrition plan tailored to the disorder by workin' with a nutritionist
Best Foot Forward
Managing emotions and mental health is just as essential as cruisin' the physical battleground. Here are a few resources for support:
- Joinin' a local or online support group for families affected by MPS disorders
- Meetin' up with other families navigatin' similar challenges through discussion forums
- Reachin' out to counseling services, hotlines, or online therapeutic resources
Don't forget to tap into the National MPS Society, an organization spillin' the beans on resources, information, and support for families affected by MPS disorders. 🌟
MPS Disorder I - Catchin' the Wind
Here's a bit more about MPS Disorder I:
MPS Disorder I - A Metabolic Elephant in the Room
MPS Disorder I, a rare genetic condition, disrupts the body's ability to metabolize sugars called glycosaminoglycans (GAGs) due to deficient or faulty alpha-L-iduronidase enzyme activity. This enzyme is vital for breaking down two GAGs, dermatan sulfate, and heparan sulfate.
The Genetic Landscape
- Autosomal Recessive Inheritance Pattern: MPS Disorder I follows an autosomal recessive genetic pattern, meaning both parents must pass a damaged IDUA gene to their child for the disorder to occur.
- IDUA Gene and Location: The defect in MPS Disorder I originates from mutations in the IDUA gene found on chromosome 4.
- Abnormal Enzyme Activity: The mutated IDUA gene results in low or absent alpha-L-iduronidase activity, leading to GAGs' accumulation in cells.
Beyond Genetics - Is There Anything Else at Play?
Although primarily caused by genetic factors, some research suggests environmental factors may play a role in the severity of MPS Disorder I symptoms. Further investigations are necessary to fully understand the extent of these factors.
MPS Disorder I - The REAL Scoop
Living a Life Swamped with MPS Disorder I
To live a manageable life with MPS Disorder I, understanding the condition is crucial. Here are some key takeaways:
- Get acquainted with healthcare specialists, including but not limited to pediatricians, geneticists, cardiologists, orthopedists, and therapists, to monitor progression and manage symptoms.
- Adopt regular exercise routines and physical therapy for mobility improvement and muscle strengthening.
- Engage with an evidence-based nutrition plan, in collaboration with a nutrition expert, to support overall health and address disorder-specific needs.
The Mind Matters, Too
- Emotional well-being is as vital as physical health. Connect with support groups, online forums, or therapeutic services to tackle emotional and psychological challenges.
- Seek appropriate education about MPS Disorder I to empower yourself and your family with valuable insights, tools, and resources.
Navigating the Medical Maze - What to Expect
To diagnose MPS Disorder I, healthcare professionals combine clinical evaluations, family histories, and laboratory tests:
- Enzyme assays to measure alpha-L-iduronidase activity
- Blood tests to pinpoint mutations in the IDUA gene
- Imaging studies like X-rays or MRIs to assess skeletal abnormalities and organ size.
Work hand-in-hand with a specialist versed in lysosomal storage disorders for comprehensive care and tailored treatment approaches.
MPS Disorder I - An Extended Look
Elevating Awareness and Support
Packed with valuable resources for families and individuals challenged by MPS Disorder I:
Healthcare Resources
Organizations like the National MPS Society provide extended knowledge, support, access to clinical trials, and information on treatment options for MPS Disorder I.
Financial Aid
These organizations offer financial relief in the form of grants, insurance navigation assistance, and fundraising resources for eligible families.
Informed Education
Educational support through tailored exercise programs, individualized education plans, and school-based accommodations can empower children with MPS Disorder I to thrive academically.
Finding Your Tribe - Connecting Locally and Online
Joining local support groups, online forums, or social media communities related to MPS disorders can provide emotional support, inspiration, and practical advice for families.
Frequently Asked Questions about MPS Disorder I
- What is MPS Disorder I?MPS Disorder I, also known as Hurler syndrome, is a rare genetic condition that alters the body's ability to break down certain sugars, causing excessive amounts to build up in cells. This disorder is part of a larger group of conditions referred to as mucopolysaccharidoses.
- What are the symptoms of MPS Disorder I?Symptoms vary but may include slow growth, distinctive facial features, joint stiffness, hearing loss, heart problems, respiratory issues, and cognitive challenges.
- How is MPS Disorder I inherited?It is inherited in an autosomal recessive manner, meaning both parents must pass a damaged IDUA gene to their child.
- Can MPS Disorder I be treated?Treatment options include enzyme replacement therapy, supportive care for developmental and physical challenges, and regular monitoring for associated health issues.
- What is the prognosis for individuals with MPS Disorder I?Prognosis is variable, with treatment and intervention contributing to better outcomes.
- Is MPS Disorder I common in children?MPS Disorder I is considered rare, with an incidence of approximately 1 in 100,000 to 1 in 200,000 live births.
- Are there any support resources available for families affected by MPS Disorder I?Yes! Organizations like the National MPS Society, educational resources, financial assistance programs, and community support groups are available for families.
"MPS Disorder I, a neurological disorder, affects the body's capacity to break down certain sugar molecules, which can trigger a variety of health complications, including chronic diseases and medical conditions such as heart problems, respiratory issues, and cognitive impairment. Understanding the underlying genetic causes can aid in early diagnosis and management, and developments like enzyme replacement therapy can help mitigate symptoms and improve the quality of life for those affected."
"Health and wellness professionals play an essential role in managing MPS Disorder I, helping individuals with the condition navigate exercise routines, evidence-based nutrition plans, and emotional support services to tackle daily challenges. A key resource for families and individuals with MPS Disorder I is the National MPS Society, which offers comprehensive information, resources, and support networks to help them better understand and cope with the disorder."